Age-dependent specifics of epidural hematoma
Specifika epidurálního hematomu v závislosti na věku
Cíl: Epidurální hematom (EDH) je potencionálně život ohrožující stav, který patří mezi traumatická poranění mozku. Léčba EDH vyžaduje včasnou diagnostiku s optimální léčbou, aby se zabránilo následnému neurologickému poškození. U dospělých pacientů klinický průběh obecně odpovídá rozsahu intrakraniální léze. U pediatrických pacientů však EDH představuje diagnostickou výzvu, a to kvůli různým vlastnostem této entity. Terapeutický přístup by proto měl být založen na klinickém stavu pacienta a na jeho individuálních potřebách. Cílem této studie bylo popsat a zdůraznit odlišné aspekty EDH u různých věkových skupin. Prezentujeme také kohortovou studii z našeho pracoviště. Materiál a metody: Do retrospektivní studie byli zařazeni dospělí i pediatričtí pacienti s rozvinutým EDH, kteří byli hospitalizováni v letech 2009–2019. Statisticky byla analyzována všechna získaná data vč. demografických údajů, mechanizmu poranění, charakteristik hematomu, souvisejících mozkových patologií, typu léčby a délky hospitalizace. Výsledky: Do studie bylo zařazeno 74 dospělých a 80 dětských pacientů. Průměrný věk u dospělých byl 42,4 let a 8,5 let u dětí. Nejčastějšími příčinami rozvoje EDH byly pády s rozdílnou etiologií. Většina dospělých pacientů byla léčena chirurgicky kvůli významnému neurologickému deficitu a dalším intrakraniálním patologiím. Dětští pacienti byli většinou léčeni konzervativně. Překvapivě nebyl rozdíl týkající se typu terapie u pediatrické skupiny tak významný, jak jsme předpokládali. Závěr: V práci jsme popsali specifika EDH u dospělých i dětských pacientů s důrazem na klinické i radiologické rozdíly. U dětí bývá často popisován indolentní průběh, i přes přítomnost významného EDH. Včasná diagnostika, optimální volba terapie a individuální přístup mohou předcházet rozvoji neurologického deficitu.
Klíčová slova:
epidurální hematom – traumatické poranění mozku – konzervativní léčba – chirurgická léčba
Authors:
B. Musilová 1; E. Brichtová 1,2; H. Valeková 1,2
Authors‘ workplace:
Faculty of Medicine, Masaryk, University, Brno, Czech Republic
1; Department of Neurosurgery, St Anne‘s University Hospital, Brno, Czech Republic
2
Published in:
Cesk Slov Neurol N 2021; 84/117(3): 269-273
Category:
Original Paper
doi:
https://doi.org/10.48095/cccsnn2021269
Overview
Aim: Epidural hematoma (EDH) is a potentially life-threatening condition that belongs to the complex of traumatic brain injuries. The management of EDH requires early diagnosis with optimal treatment to prevent subsequent neurological impairment. In adults, the clinical course generally corresponds to the extent of an intracranial lesion. However, in pediatric patients, EDH represents a diagnostic challenge due to the different features of this entity. Therefore, the therapeutic approach should be based on the patient‘s clinical status and individual requirements. The aim of this study was to describe and highlight the different aspects of EDH in the various age groups. We also present a cohort study from our hospital. Materials and methods: Adult and pediatric patients admitted to the hospital between 2009 and 2019 with developed EDH were retrospectively reviewed. All data including demographic information, mechanism of injury, characteristics of hematoma, associated brain pathologies, treatment, and duration of hospitalization were acquired and statistically analyzed. Results: Seventy-four adult and eighty pediatric patients were included. The mean age in the adult group was 42.4 years and 8.5 years in the pediatric group. The most common causes of EDH were falls of different etiologies. The majority of adult patients were managed surgically due to significant neurological deficits and other cranial pathologies. Pediatric patients were predominantly treated conservatively. Surprisingly, the difference regarding the type of therapy was not as significant in the pediatric group as we assumed. Conclusion: We described specific features of EDH in adult and pediatric patients with emphasis on clinical and radiological differences. In children, the indolent course is often described, despite the presence of significant EDH. Early diagnosis, optimal choice of therapy, and individual approach can prevent the development of neurological deficits.
Keywords:
epidural hematoma – traumatic brain injury – conservative therapy – surgical therapy
Introduction
Traumatic brain injury (TBI) is a wide group of conditions negatively affecting the brain tissue with disruption of its proper function [1]. Epidural or extradural hematoma (EDH) is a type of TBI. The prevalence of developing EDH is about 2–3% of all pediatric neurotraumas [2,3] and about 2.7–4% of adult cases [4]. Despite the improvement of neurotrauma care, EDH is still a severe disorder with relatively high morbidity and mortality [4,5]. Overall mortality varies across studies, where the range is about 0–12% in the pediatric group [2] and about 1.2–33% in the adult group [4,6]. However, in the majority of cases the impact on neural function is reversible if diagnosed early and managed carefully. Pediatric EDH represents a diagnostic challenge due to dissimilar features compared to adult patients [3]. In adults, the occurrence of EDH is usually between 20 and 30 years [4], in children between 6 and 10 years, and strong male predominance is described in both groups [3].
Several age-specific characteristics have been observed in clinical practice regarding the method of injury, clinical presentation, CT image, and type of treatment. Adult patients usually present with severe neurological dysfunction due to conjoined intracranial lesions. On the contrary, neurological deterioration tends to be expressed less in younger patients [3] considering the flexibility of the dura mater and the plasticity of brain tissue. The typical CT image of EDH is described as the lens-shaped hyperdense collection of blood above the dura mater without crossing the sutures (in 84% of cases) [4,7]. However, in pediatric patients, the shape of the hematoma often resembles a subdural hematoma. Etiology along with the type of treatment varies in pediatric and adult patients in view of actions accompanied by injury, associated brain injury such as contusion, fractures, etc. and the comorbidities’ influence on older patients. Despite the diagnostic process being the same, every patient is unique and requires a specific and individualized approach [3,8].
Materials and methods
Our study was designed as a retrospective, cohort study. We focused on adult and pediatric patients with diagnosed EDH who were treated between 2009 and 2019. The population from which the hospital admits the patients includes approximately 1.8 million residents; however, the influence of other hospitals may be reflected. Regarding the pediatric groups, all patients from the selected region are usually directed to the mentioned hospital. All data were acquired from the hospital database with an emphasis on the etiology of the injury, localization of EDH, method of therapy (surgical vs. conservative), and the duration of hospitalization. In addition, standard epidemiological data including age and sex ratio were reviewed. On the basis of the initial CT scan, we determined the localization of the he- matoma and associated brain injuries. According to the therapy, patients were divided into groups treated surgically using craniotomy or craniectomy and patients without any surgical intervention. Statistical analysis was then performed with Basic statistical tests, MS Excel (Microsoft, Washington, USA).
Results
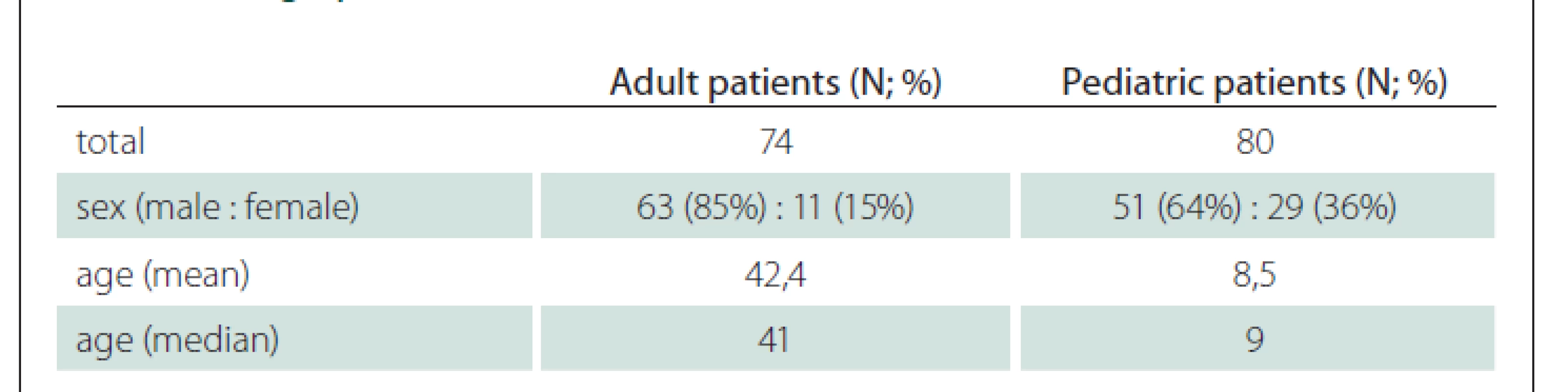
In total, 74 adult patients and 80 pediatric patients were included in our retrospective study. In both groups there was a significant male-to-female predominance. The average age for developing injury in adults was 42.4 years (Tab. 1). Among adult patients, accidental falling comprised of about 50% of all EDH cases (overall 39 patients). In total, 16 cases of falls were associated with alcohol abuse. Road traffic accident presented in the second place (12 patients) and falls from heights (7 patients) occupied the third place (Tab. 2a). Based on the neurological status and CT findings, 61 patients were managed surgically and 13 patients were observed only. Three patients were admitted with severe neurological deterioration due to associated cranial injuries, therefore they were treated by decompressive craniectomy (Tab. 3a). Regarding the origin of EDH (middle meningeal artery), the most common region of hematomas was in the temporal and temporo-parietal area. The extent of treatment was adapted to the extent of cranial pathologies. In patients with fractures of the skull base, other types of hemorrhage, and lower values of Glasgow Coma Scale, the therapeutic approach was more aggressive with a correspondingly longer duration of hospitalization (Fig. 1, 2). On the contrary, in patients presenting with the minimal neurological status changes and minor EDH, less invasive therapeutic modality was preferred (Fig. 3).




Obr. 1. CT mozku, axiální řez. Dospělý
pacient s epidurálním hematomem
– chirurgické řešení (další přidružená
poranění).

Obr. 2. CT mozku, axiální řez. Dospělý
pacient s epidurálním hematomem –
chirurgické řešení (objemný epidurální
hematom).

Obr. 3. CT mozku, axiální řez. Dospělý
pacient s epidurálním hematomem –
konzervativní postup.

In the pediatric group, the mean average age was 8.5 years (Tab. 1). Similarly to other studies [3,4,9], falling represented the highest incidence (25 patients) as in the adult cohort. More specifically, falling was associated with normal children’s activities (swinging, playing, walking, running, etc.). A road traffic accident was the second most frequent reason of EDH development. Pediatric patients were involved in car accidents in the co-rider’s role (19 patients) or were hit by a car (6 patients). The third place was reserved for falling from heights (15 patients), most often associated with climbing a tree (Tab. 2b). According to the localization, hematomas occurred frequently in the temporal (17 patients), parietal (17 patients), frontal (13 patients), or temporo-parietal region (15 patients). In addition, in five pediatric patients, the hematoma was localized in the posterior fossa; this condition is typical for younger patients (Tab. 2b). Thirty-nine patients required surgical treatment. Generally, these patients were admitted with a more severe neurological impairment or there was another intracranial lesion present (Tab. 3b). Fig. 4 illustrates one of the candidates for surgical treatment. Interestingly, conservative therapy was only slightly predominant in children (41 patients). These hematomas were minor with minimal change in the neurological status (Fig. 5).
Obr. 4. CT mozku, axiální řez. Pediatrický
pacient s epidurálním hematomem
– chirurgické řešení (objemný epidurální
hematom).

Obr. 5. CT mozku, axiální řez. Pediatrický
pacient s epidurálním hematomem – konzervativní
postup.

The duration of hospitalization was longer in general in adult patients based on usage of a more aggressive approach. Delayed discharge in pediatric patients was usually as- sociated with conservative therapy due to a more accurate observation or adjacent cranial trauma (Tab. 4).

Discussion
Our results have shown that the etiology of EDH is similar in children and in adults. In both groups we observed that falling accidents with different origins represented the primary cause of developed EDH. The majority of injuries in adult patients were associated with alcohol abuse, but in pediatric patients the majority of falls were associated with swinging, playing or climbing a tree. Important aspect that can influence the clinical status and following outcome is the absence of additional comorbidities, e. g., arterial hypertension, diabetes, alcohol abuse, etc. in pediatric patients. As these risk factors may have a negative impact on the prognosis in older patients, in children a more favorable outcome is reported with a higher probability of rapid and complete recovery [8]. Concurrent traumatic brain injuries, e. g., subdural hematoma, subarachnoid hemorrhage, intracerebral hematoma, and fractures were noticed mainly in older patients leading to a more unfavorable neurological resolution. Generally, subdural, subarachnoid, or intracerebral hemorrhage tends to occur more often than EDH in adult patients [7].
Regarding the clinical presentation, the literature typically mentions a lucid interval which is particularly expressed in adults. However, clinical studies describe this unique phenomenon only in 50% of patients. The lucid interval is characterized as a state of consciousness between initial unconsciousness and delayed neurological deterioration [4]. Generally, children present with non-specific symptoms – mild headache, fatigue, drowsiness, malaise, vomiting, short-term unconsciousness, etc. and an absence of the lucid interval. In our cohort the lucid interval was presented in 5 pediatric patients (6.3%) and in 14 adult patients (19%), but this can be significantly influenced by the medical history taking, associated injuries and also the overall neurological status of the patients. On the other hand, the complete absence of symptoms is also possible, therefore the diagnosis becomes more complicated and challenging. In addition, children are usually unable to explain or describe the exact manner of the injury. Physicians should be aware of a possibility of EDH or other intracranial pathologies even if the patient is asymptomatic and refers to a trivial injury [7]. A positive correlation was described between the outcome and the severity of the clinical course. If symptoms are significantly expressed, the child’s relatives are seeking medical care earlier and the following evaluation is more active [10]. Another important exception should be mentioned – absence of the grey zone in the youngest patients. In practice, it includes excessively rapid progression from the originally stable clinical condition to the loss of consciousness. On the contrary, in adults, the progression is typically gradual with the possibility to intervene in time to prevent consequences.
Epidural hematoma occurs in 85% of cases due to a ruptured medial meningeal artery as a consequence of skull fracture. Other sources of bleeding include diploic veins in association with the high vascularity of diploic or dural venous sinuses, mainly in children. The absence of the bony groove for the medial meningeal artery in younger patients is assumed as the reason for different sources of bleeding regarding age [4,8]. In infants, the formation of EDH is described very rarely due to high compliance of cranial bones with a strong attachment of the dura mater [2,7,8,11]. Especially in younger patients, the source of bleeding may affect the clinical course. The venous circulation is a low-pressure system, therefore the filling of the epidural space with the following brain tissue compression will be gradual with a corresponding delayed onset of symptoms [12]. A similar principle defines the appearance of the CT image. In pediatric patients, less extensive hematoma with the absence of a typical lens-shape is often expressed due to more elastic features of the dura mater. The supratentorial localization is predominant in both groups, where the parietal and frontal regions are affected predominantly in the pediatric group and the temporal area in the adult group [7]. EDH tends to occur more frequently in the right hemisphere [13]. In very rare cases, simultaneous supra- and infratentorial EDH can occur [14]. EDH in the posterior fossa is described notably in pediatric patients due to ruptured dural venous sinuses [4]. In any case, the trauma mechanism should be carefully investigated and considered in the context of the clinical image and presumed as a type of traumatic brain injury.
Optimal treatment is essential for the following outcome. Surgical or conservative treatments are the main therapeutic approaches and both can provide an acceptable outcome if carefully evaluated [7]. In adults, there are often other associated traumatic brain injuries, hence the treatment is quite aggressive. The type of surgical intervention is based on the neurological status of the patient, initial CT scan (extent of hematoma, midline shift, ventricular compression due to brain edema), and other patient specific parameters [15]. It is recommended to perform a craniotomy which enables the surgeon to overlook the epidural space with possible coagulation of the bleeding source [16]. If the localization of hematoma is vaguely defined according to the CT image, performing a small durotomy may ensure that the blood is not located in the subdural space. Ultimate method is a decompressive craniectomy, which was used in three cases in our cohort due to the presumption of intracerebral pressure increase with a progression of brain edema. The trephination is saved for chronic cases due to insufficient brain exposure with a limited possibility of treating the bleeding source.
In pediatric patients, EDH is often a self-limited disease. The management of pediatric EDH is usually conservative including intensive observation during hospitalization. In the case of neurological decline, repeated CT imaging could help to exclude a hematoma expansion or delayed hematoma formation [16]. Nevertheless, controversy exists about repeating radiological examination due to higher exposure to radiation with a subsequent negative impact on the developing neuronal tissue [17]. In adults, performing repeated CT scans after 4–8 hours is an usual part of the diagnostic protocol in neurotrauma.
Generally, there are many controversies about the efficiency of surgical treatment in children due to lack of parameters precisely indicating patients for operative and non-operative procedures [11,18]. In addition, more consistent observation requires a longer duration of hospitalization.
Despite available evidence-based recommendations for the optimal treatment of traumatic brain injury [19], each patient presents an individual challenge. Therefore, physicians have to use both personal skills and theoretical knowledge to correctly evaluate the benefits of either a surgical or conservative approach.
We are aware of some limitations of our study – small cohort, retrospective design, and absence of standardized guidelines. Therefore, our data are non-homogenous and indications for surgical treatment are based only on our experience. Globally, a need for standard therapeutic guidelines for pediatric and adult EDH treatment is required.
Conclusion
Our results illustrate the specific features of EDH depending on the age of patients. In children, the clinical course tends to be inconspicuous due to the smaller size of the hematoma and vague CT findings. Therefore, physicians should be cautious about every child without significant improvement after a mild head injury. However, potentially extensive brain plasticity allows children to achieve a more favorable outcome. Pediatric patients are often candidates for non-operative treatment considering the absence of comorbidities and associated injuries. Adult patients with associated traumatic brain injury and poor admission status require aggressive surgical therapy which can provide an option to overlook the epidural space with elimination of the bleeding source. The final outcome is often influenced by concurrent comorbidities. Generally, standardized therapeutic guidelines are utilized, but physicians should consider each case individually by providing the most suitable therapeutic approach.
Ethical priciples
The entire study was conducted in accordance with the Helsinki Declaration of 1975 (as revised in 2004 and 2008). For this type of study, formal consent is not required. Informed consent was obtained from all individual participants included in the study.
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers‘ bureaus; memberships, employment, consultancies, stock ownership, other equity interest; and expert testimony or patient-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Assist. Prof. Eva Brichtová, MD, PhD
Department of Neurosurgery St Anne‘s University Hospital Pekařská 664/53 656 91 Brno Czech Republic
e-mail: eva.brichtova@fnusa.cz
Accepted for review: 4. 2. 2021
Accepted for print: 3. 6. 2021
Sources
1. Ghajar J. Traumatic brain injury. Lancet 2000; 366(9233): 923–929. doi: 10.1016/ S0140-6736(00)02689-1.
2. Binder H, Majdan M, Tiefenboeck TM et al. Management and outcome of traumatic epidural hematoma in 41 infants and children from a single center. Orthop Traumatol Surg Res 2016; 102(6): 769–774. doi: 10.1016/ j.otsr.2016.06.003.
3. Bounajem MT, Samples DC, Wallace DJ et al. Management of epidural hematomas in pediatric patients presenting with a GCS of 14 or better. J Clin Neurosci 2019; 70: 118–122. doi: 10.1016/ j.jocn.2019.08.056
4. Almeida de LP, Casarin MC, Rogério LP et al. Prognostic factors trauma and epidemiologic related in surgically treated extradural hematoma. J Surg Res 2019; 2(3): 105– 115. doi: 10.26502/ jsr.10020026.
5. Svoboda N, Tyll T, Beneš V et al. Epidural hematoma – benign or potentially malignant disease? Rozhl Chir Spring 2018; 97(6): 267–272.
6. Soon WC, Marcus H, Wilson M. Traumatic acute extradural hematoma – indications for surgery revisited. Br J Neurosurg 2016; 30(2): 233–234. doi: 10.3109/ 02688697.2015.1119237.
7. Al-Mamoori MJ. Management of epidural hematoma in the pediatric age group. Med J Babylon 2019; 16(4): 276–285. doi: 10.4103/ MJBL.MJBL_47_19.
8. Rocchi G, Caroli E, Raco A et al. Traumatic epidural hematoma in children. J Child Neurol 2005; 20(7): 569–572. doi: 10.1177/ 08830738050200070501.
9. Zhang F, Huang L, Singichetti B et al. Sex and age differences in hospitalised pediatric traumatic brain injury. Pediatr Int 2019; 61(9): 904–912. doi: 10.1111/ ped.13946.
10. Kandregula S, Sadashiva N, Konar S et al. Surgical management of traumatic extradural hematomas in children: an analysis of 201 patients at a tertiary neurosurgical center. Childs Nerv Syst 2019; 35(5): 807–813. doi: 10.1007/ s00381-019-04088-1.
11. Atci IB, Yilmaz H, Yaman M et al. Incidence, hospital costs and in-hospital mortality rates of surgically treated patients with traumatic cranial epidural hematoma. Roman Neurosurg 2017; 4: 510–516. doi: 10.2478/ romneu-2018-0013.
12. Jamous MA. The outcome of observation of acute traumatic extradural haemorrhage in pediatric age group. Eur J Trauma Emerg Surg 2021; 47(3): 847–853. doi: 10.1007/ s00068-019-01262-7.
13. Faheem M, Jaiswal M, Ojha BK et al. Traumatic pediatric extradural hematoma: an institutional study of 228 patients in tertiary care center. Pediatr Neurosurg 2019; 54(4): 237–244. doi: 10.1159/ 000501043.
14. Nasi D, Iaccarino C, Romano A et al. Surgical management of traumatic supra and infratentorial extradural hematomas: our experience and systematic literature review. Neurosurg Rev 20202; 43(3): 893–901. doi: 10.1007/ s10143-019-01083-7.
15. Maugeri R, Anderson DG, Graziano F et al. Conservative vs. Surgical management of post-traumatic epidural hematoma: A case and review of literature. Am J Case Report 2015; 16: 811–817. doi: 10.12659/ AJCR.895231.
16. Zwayed AR, Lucke-Wold B. Conservative management of extradural hematoma: a report of sixty-two cases. Neurol Clin Neurosci 2018; 2(2): 5–9.
17. Samples DC, Bounajem MT, Wallace DJ et al. Role of follow-up CT scans in the management of traumatic pediatric epidural hematomas. Childs Nerv Syst 2019; 35(11): 2195–2203. doi: 10.1007/ s00381-019-04236-7.
18. Flaherty BF, Moore HE, Riva-Cambrin J et al. Pediatric patients with traumatic epidural hematoma at low risk for deterioration and need for surgical treatment. J Pediatr Surg 2017; 52(2): 334–339. doi: 10.1016/ j.jpedsurg. 2016.09.005.
18. Guidelines for the Management of Pediatric Severe TBI, 3rd ed. Guidelines for the Management of Severe TBI, 4th ed. [online]. Available from URL: https:/ / www.braintrauma.org/ coma/ guidelines.
Labels
Paediatric neurology Neurosurgery NeurologyArticle was published in
Czech and Slovak Neurology and Neurosurgery

2021 Issue 3
Most read in this issue
- Developmental dysphasia – functional and structural correlations
- Guidelines on intravenous thrombolysis in the treatment of acute cerebral infarction – 2021 version
- Ethylenglycol poisoning
- Surgical treatment possibilities of drug-resistant Ménière‘s disease
