Correlation between self-esteem and self-compassion in patients with multiple sclerosis – a cross-sectional study
Korelace mezi sebeúctou a soucitem vůči sobě u pacientů s roztroušenou sklerózou – průřezová studie
Cíl: Tato studie byla provedena s cílem stanovit vztah mezi sebeúctou a soucitem vůči sobě u pacientů s RS. Metody: Tato deskriptivní studie byla provedena na 51 pacientech s RS z několika měst v Íránu. Pacienti byli vybíráni pomocí dostupné metody vzorkování. Pro sběr dat byly u pacientů s RS použity standardní nástroje pro hodnocení sebeúcty a nástroje vytvořené výzkumníky pro hodnocení soucitu vůči sobě. Data byla analyzována pomocí Pearsonova korelačního koeficientu a softwaru SPSS, verze 20. Výsledky: Průměrný věk účastníků studie byl 36,54 let. Většina účastníků byly vdané ženy. Při soucitu k sobě výsledky ukázaly pouze statisticky nevýznamnou korelaci mezi sebeúctou a mírou laskavosti k sobě (r = 0,205), sebehodnocením (r = 0,024), celkovým smyslem pro lidskost (r = 0,111), uvědomělostí (r = 0,24), hledáním podpory (r = 0,145) a tím, že je daný člověk vzorem pro ostatní (r = 0,57) (ve všech případech p > 0,05). Závěr: Poskytnutím vhodných řešení pro zvýšení sebeúcty pacientů s RS a jejich soucitu k sobě samým, u nich dojde ke korekci a zlepšení kvality duševního a nakonec i fyzického stavu.
Klíčová slova:
soucit vůči sobě – roztroušená skleróza – sebeúcta – korelace
Authors:
H. Dahmardeh 1; A. Sadooghiasl 2; E. Mohammadi 2; A. Kazemnejad 3
Authors‘ workplace:
Ph. D. Student, Department of Nursing, Faculty of Medical Sciences, Tarbiat, Modares University, Tehran, Iran
1; Department of Nursing, Faculty, of Medical Sciences, Tarbiat Modares, University, Tehran, Iran
2; Department of Biostatistics, Faculty, of Medical Sciences, Tarbiat Modares, University, Tehran, Iran
3
Published in:
Cesk Slov Neurol N 2021; 84/117(2): 169-173
Category:
Original Paper
doi:
https://doi.org/10.48095/cccsnn2021169
Overview
Aim: This study was performed to determine the correlation between self-esteem and self-compassion in patients with MS. Methods: This descriptive study was performed on 51 patients with MS from multiple cities of Iran. Patients were selected through available sampling method. Standard self-esteem tools and self-compassion researcher-made tools were used in patients with MS in order to collect data. Data were analyzed using the Pearson correlation coefficient and SPSS software version 20. Results: The mean age of participants was 36.54 years. Most of the participants were women and married. The results showed only statistically insignificant correlation between self-esteem and dimensions of self-kindness (r = 0.205), self-judgment (r = 0.024), common sense of humanity (r = 0.111), mindfulness (r = 0.24), seeking support (r = 0.145) and being a model for others (r = 0.57) in self-compassion (P > 0.05 in all cases). Conclusion: Providing appropriate solutions to increase self-esteem and self-compassion in these patients will cause to correct and improve the quality of mental and ultimately physical condition of these patients.
Keywords:
self-compassion – Multiple sclerosis – self-esteem – correlation
Introduction
Today, MS is considered to be one of the major management challenges in chronic diseases in the world. According to the latest Global Burden of Disease report, more than 2,188,221 people in the world have MS, which indicates an increase of 10% compared to 1990 [1]. Therefore, according to the latest information, in 2019, there are more than 36,287 patients with MS in Iran [2].
Multiple sclerosis is the most common inflammatory neurological disorder, especially in young people [3]. Due to its greater impact on young people as an economically active population, MS causes irreparable effects on the lives of individuals, families and communities [4]. MS leads to affect the psychological dimensions and reduce the quality of life in these patients due to the increasing complications of drugs or disease progression as well as having long-term complications (muscle spasms, paralysis especially in the legs, urological problems, sexual dysfunction, and mental disorders) [5,6]. MS causes increased anxiety, depression, stress, fatigue and long-term suffering in these patients [7–9]. Existing therapies for the treatment of psychological complications are drugs that, in addition to many long-term benefits, cause various complications, such as sleep disorders and gastrointestinal complications [10]. Psychiatric complications in MS patients cause emotional and psychological responses in them [11].
Numerous factors, including self-compassion, affect how people respond emotionally to distressing events [12]. Self-compassion is an adaptive way of communicating with oneself when a person becomes aware of incompetence and encounters difficult situations in life, such as interpersonal problems, leaving behind trauma and natural disasters, and chronic diseases and causes a person to have a cautious and non-judgmental view of oneself, including failures and in-competencies [13]. Self-compassion is associated with lower depression and higher negative emotions and mental health. Self-compassion provides all the benefits of high self-esteem, such as higher mental well-being and better overall adaption without problems. But self-compassion is not the same as self-esteem. However, in case of low self-esteem, it is difficult to increase self-compassion and lack of compassion is related to low well-being and self-esteem [14].
Severe stress associated with chronic diseases can significantly reduce a person‘s self-esteem, and people are prone to low self-esteem during the course of a chronic disease due to sense of loss of control over many issues related to their health and the complications caused by the disease. If patients with MS also have lower level of self--esteem, this matter can lead to decreased life satisfaction, increased prevalence of depression and other physical diseases [15]. This is why people with high self-esteem have a high sense of empowerment and value and ensure that their efforts will lead to a result and they see most of the good aspects of the issues and do their best effort to take control of the disease and overcome it. A review of studies also confirms that people with higher self-esteem are more resistant to life issues, problems, and psychological stresses than people with low self-esteem, and as a result, they are more likely to succeed in doing works [16,17].
Neff stated that although these two components (self-compassion and self-esteem) are distinct and separate from each other, it is expected that self-compassion and self--esteem are related to each other, so that people with low self-compassion should have less self-esteem due to their extreme judgment, a sense of isolation and excessive identity with negative thoughts and feelings. Conversely, people with high self-compassion should have more self-esteem due to their kind behavior and mental reminder that incompetency is part of the human conditions [18].
However, since self-compassion is a context-dependent trait and influenced by norms, values, and procedures of group, and studies show that the level of self-efficacy vary across different cultures, the findings of Neff et al [19] indicate different levels of self-compassion in Taiwan and Thailand as Asian countries than in the United States, and this concept (of self--compassion) is considered as a value that these values are chosen by individuals, change and vary from person to person, and how people respond to stressful and painful situations is affected by them, and self-esteem means a sense of self-worth. This feeling comes from a set of thoughts, feelings, emotions and experiences during life [19–21].
It seems that there are different methods in understanding the concepts of self-esteem and self-compassion in different patients that affect how these concepts are related. Also, a correct understanding of these concepts can help patients and health staff to better adapt to the disease in the long-term. Therefore, this study was carried out to investigate the correlation between self-compassion and self-esteem in patients with MS.
Methods
Design and participants
This cross-sectional study was performed on 51 patients with MS referred to MS associations in Zahedan, Ahvaz, Kerman, East Azerbaijan, Ardabil, Yazd, Fasa, Astara, Amol, Sabzevar and North Khorasan in Iran from January 10 to July 20, 2020. Participants were selected through the convenience sampling method. The inclination criteria included patients with known MS who had been diagnosed at least for 6 months, aged between 18–50 years, without any drug addiction, having minimum literacy, ability to respond to questionnaire questions, no hearing impairment (if he/ she is not able to fill in the questionnaire, someone else will read it to him/ her and the patient will express his/ her opinion), patients who are not in the acute phase of MS, and without any disease and any acute or chronic mental disease such as severe depression and forgetfulness. The exclusion criteria were unwillingness to continue to participate in the study for any reason, causing complications, known serious mental disorders and a disease during the study (mental disorders including major depression or bipolar disorder), the occurrence of a stressful event in life that causes to disrupt a person‘s psychological balance like the death of a loved one.
Data collection
First, the researcher, after obtaining official permission from the University Ethics Committee, obtained the necessary letter of introduction to enter the research environment of MS associations in the cities where the research was carried out. In this way, the questionnaire was designed electronically and provided to the MS associations and the presidents of the associations, and after their approval in terms of the quality of the questionnaires and the ability of patients to respond to them, it was provided to patients who are members of the associations (Associations of Zahedan, Ahvaz, Kerman, East Azerbaijan, Ardabil, Yazd, Fasa, Astara, Amol, Sabzevar and North Khorasan) to be completed.
Tools
The data collection tools included a questionnaire of personal characteristics (age, sex, field of study, marital status, and place of residence) and Rosenberg self-esteem scale (RSES) and a self-compassion researcher-made questionnaire.
Rosenberg self-esteem questionnaire
This is a standard 10-item questionnaire developed by Rosenberg in 1965 that identifies a person‘s general feeling about self-esteem. Answering the questions is based on a four-point Likert scale, with scoring range is from zero to three scores including: strongly disagree (0), disagree (1), agree (2) and strongly agree (3), where a score of 30 is the highest score. Scores > 25 indicate high self-esteem, scores 15–25 indicate moderate self-esteem, and scores < 15 indicate low self-esteem [22]. The reliability of this tool was confirmed in the study performed by Pullman and Allik with a correlation coefficient of 0.91 [23]. RSES reliabity and validity was approved by Shapurian et al [24].
Self-compassion researcher-made questionnaire
This questionnaire has 73 items and measures self-compassion in 11 dimensions including self-kindness, self-judgment, common sense of humanity, isolation, mindfulness and over-identification, seeking support, concealment, spiritual resilience, and being a model for others, worrying about cohabitation in patients with MS with five-point Likert scale (always, most often, often, rarely and never).
Statistical analysis
SPSS V20 software (IBM, Armonk, NY, USA) was used for data analysis. Descriptive (mean, percentage, frequency) and analytical (chi-square) tests were used. The significance level was considered lower than 0.05.
Results
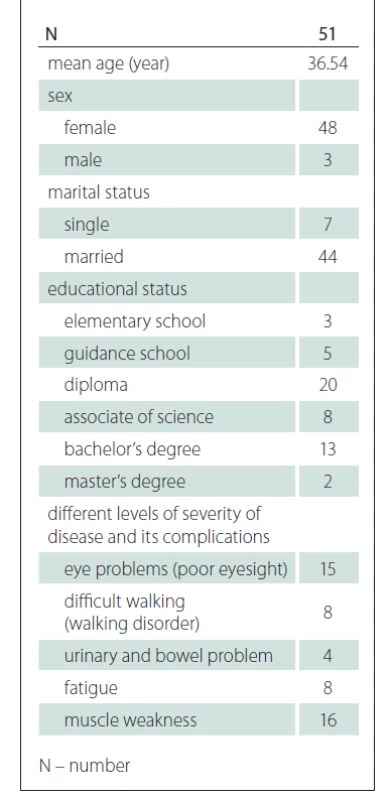
Characteristics of study population is presented in Tab. 1.
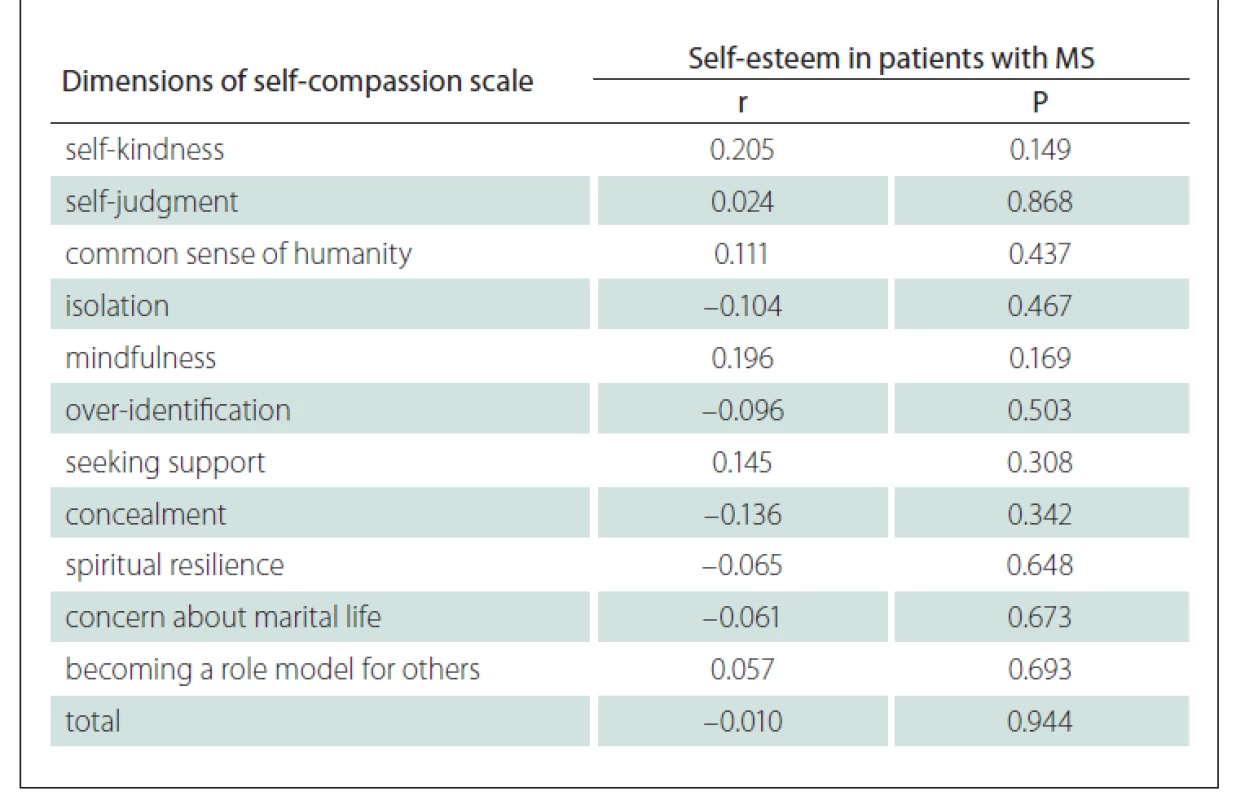
According to the Pearson correlation test, only statistically insignificant direct correlation was observed between self-esteem and the dimensions of self-kindness, self-judgment, common sense of humanity, mindfulness, seeking support and being a model for others and, statistically insignificant indirect correlation between self-esteem and dimensions of isolation, over-identification, concealment, spiritual resilience and concern about marital life. The Pearson correlation coefficient with the whole questionnaire was also not significant (Tab. 2).
Discussion
The aim of this study was to determine the correlation between self-esteem and self-compassion dimensions in patients with MS.
The results of the presented study showed that self-kindness, common sense of humanity, and mindfulness were directly related to self-esteem. It was shown that people with self-compassion (people who have compassionated toward themselves) had many psychological strengths, such as greater happiness and optimism [20]. These three dimensions of self-compassion are adaptive in nature and show that if a person experiences a negative life, the person’s approach to oneself is warm, gentle, and kind, and in this way, a person can experience more positive and less negative feelings [25]. According to the results of the presented study, another dimension with direct relationship to self-esteem is self-judgment. Internal stigma is a form of self-judgment and occurs when people internalize society’s negative views toward themselves. Internalized stigma affects people’s perceptions of themselves and thus leads to blame and guilt [26]. However, a patient with a chronic disease such as MS may hide his or her illness from others to avoid the stigma. This issue is also related to the dimension of concealment, which according to the results of the presented study has an indirect relationship to self-esteem. Joachim and Acorn showed that patients with chronic diseases with visible or invisible symptoms hid their disease from others for various reasons such as stigma and isolation, and patients with MS who have both visible and invisible symptoms were no exception to this rule and tried to hide their disease [27]. And it seems that since the questionnaires were distributed electronically among the patients and the researcher did not have face-to-face communication with the patients, these patients tried to hide their disease from others and thus had less self-judgment and as a result, this component has a direct relationship with self-esteem. Other dimensions of self-compassion that are directly related to self-esteem are seeking support and being models for others, both of which require acceptance and social support from the point of view of other people and their peers and family.
Social support can be described as social and psychological support provided by the environment. The individual social support system includes peers, friends and family members, and among them, the family and peers are the most important sources of social support. A person’s psychological growth starts in the family, but later on, peers become important. Acceptance by peers positively affects self-acceptance and self-confidence. An adolescents’ self-esteem, which is loved, admired and accepted by their peers, will also cause positive growth. A person with low self-esteem believes that important people, especially his parents, do not like and do not appreciate him. For this reason, it can be assumed that there is a direct relationship between self-esteem and social support [28].
If this issue is also seen in patients with MS and they seek support from family or treatment team, the findings of Harris et al [29], in line with the results of the presented study, showed that there was a direct relationship between individuals’ social status and level of self-esteem and their relationship was reciprocal at all stages of the development throughout life. Also, Arslan [28] in his study showed that there was a direct and significant relationship between self-esteem and social support received from family and teachers.
According to the results of the presented study, it was found that the dimensions of isolation and over-identification had an indirect relationship with self-esteem. These dimensions of self-compassion mean that the person attributes mistakes and failed life experiences to his/ her performance, and strongly recognizes negative emotions when faced with failure. Isolation and over-identification involve negative evaluation of the person and feelings when experiencing a stressful and painful event. Therefore, these dimensions of self-compassion are inconsistent.
One of the other dimensions of self-compassion, which has an indirect relationship with self-esteem in patients with MS, is spiritual resilience [30]. Spiritual resilience is the ability to maintain feelings and goals through a set of beliefs, principles, or values using internal and external spiritual resources when faced with pressure, stress, and trauma [20]. Borji et al [31] suggested self-esteem as a mediator between spiritual health and resilience and stated that since spiritual and religious beliefs were important issues in the lives of Iranians, the field of self-esteem could be strengthened through spirituality education and increased positive attitude towards life [31]. The results of their study contradict the presented study.
Another dimension of self-compassion, which has an indirect relationship with self-esteem in patients with MS, is worrying about cohabitation [32]. When physical health is impaired in a chronic disease, patients’ interactions with their relatives and partners are severely affected, and they become concerned about their cohabitation and this leads to decrease their self-esteem. Consistent with the results of the presented study, the results of a study by Erol et al [33] showed that high self-esteem was beneficial in romantic relationships. In addition, research using data from both partners showed that high self-esteem also had a positive effect on the partner’s happiness in the relationship. Finally, in general, self-esteem indirectly correlates with self-compassion dimensions. This may be because MS has a great negative effect on patients’ self-esteem by causing cognitive and psychological changes. Self-compassion is also more changeable than self-esteem, which is difficult to increase if self-esteem is low [14].
The most important limitation of the presented study is a descriptive character of the study that should be considered when interpreting the results. Another limitation is a low sample size, which was partly due to the study time during the COVID-19 pandemic, which resulted in fewer visits and less access to patients. Despite the mentioned limitations, this study also has some advantages, including the fact that limited studies were performed so far on this topic and on patients in different cities.
Conclusion
Self-esteem and self-compassion are two independent structures, but self-esteem is directly related to some dimensions of self - compassion, and by planning to maintain and promote self-esteem, self-compassion can be maintained or enhanced in these dimensions, thus helping the individual to take advantage of self-compassion. In the dimensions that were indirectly related to self-esteem, these aspects, which are often negative aspects of self - compassion, can also be reduced by strengthening self-esteem. Therefore, it can be expected that providing appropriate solutions such as the implementation of effective educational programs and psychological counseling to increase self-esteem in patients with MS may improve the mental state of these patients to reduce the complications, problems and high costs of care and treatment of their disease and ultimately lead to an increase in the general health of MS patients.
Ethical principles
This study has been registered by the Ethics Committee of Tarbiat Modares University, Medical School with ethics code: IR.MODARES.REC.1398.139. All participants provided written consent. STROBE checklist was used to report the study [24].
Conflict of interest
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
Acknowledgement
This study is part of a PhD thesis of the first author. All authors as well as all participants of this study would like to express their gratitude to Tarbiat Modares University.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Afsaneh Sadooghiasl
Department of Nursing
Faculty of Medical Sciences
Tarbiat Modares University
P.O.BOX.14115-331 Tehran, Iran
e-mail: a.sadooghi@modares.ac.ir
Sources
1. Wallin MT, Culpepper WJ, Nichols E et al. Global, regional, and national burden of multiple sclerosis 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019; 18(3): 269–285. doi: 10.1016/ S1474-4422(18)30443-5.
2. Hosseinzadeh A, Baneshi M, Sedighi B et al. Incidence of multiple sclerosis in Iran: a nationwide, population-based study. Public Health 2019; 175 : 138–144. doi: 10.1016/ j.puhe.2019.07.013.
3. Hauser SL, Cree BA. Treatment of multiple sclerosis: a review. Am J Med 2020; 133(12): 1380–1390. doi: 10.1016/ j.amjmed.2020.05.049.
4. Paz-Zulueta M, Parás-Bravo P, Cantarero-Prieto Det al. A literature review of cost-of-illness studies on theeconomic burden of multiple sclerosis. Mult Scler Relat Disord 2020 : 102162. doi: 10.1016/ j.msard.2020.102162.
5. Kan FP, Hoseinipalangi Z, Ahmadi N et al. Global, regional and national quality of life in patients with multiple sclerosis: a global systematic review and meta-analysis. BMJ Support Palliat Care 2020 [ahead of print]. doi: 10.1136/ bmjspcare-2020-002604.
6. Yazgan YZ, Tarakci E, Tarakci D et al. Comparison of the effects of two different exergaming systems on balance, functionality, fatigue, and quality of life in people with multiple sclerosis: a randomized controlled trial. Mult Scler Relat Disord 2020; 39 : 101902. doi: 10.1016/ j.msard.2019.101902.
7. Leavitt VM, Brandstadter R, Fabian M et al. Dissociable cognitive patterns related to depression and anxiety in multiple sclerosis. Mult Scler 2020; 26(10): 1247–1255. doi: 10.1177/ 1352458519860319.
8. Tobore TO. Oxidative/ nitroxidative stress and multiple sclerosis. J Mol Neurosci 2021; 71(3): 506–514. doi: 10.1007/ s12031-020-01672-y.
9. Manjaly ZM, Harrison NA, Critchley HD N et al. Pathophysiological and cognitive mechanisms of fatigue in multiple sclerosis. J Neurol Neurosurg Psychiatry 2019; 90(6): 642–651. doi: 10.1136/ jnnp-2018-320050.
10. Montalban X, Gold R, Thompson AJ et al. ECTRIMS/ EAN guideline on the pharmacological treatment of people with multiple sclerosis. Mult Scler 2018; 24(2): 96–120. doi: 10.1177/ 1352458517751049
11. Madan S, Pakenham KI. The stress-buffering effects of hope on adjustment to multiple sclerosis. Int J Behav Med 2014; 21(6): 877–890. doi: 10.1007/ s12529-013-9384-0.
12. Amanelahi A, Tardast K, Aslani K. Prediction of depression based on components of self-compassion in girl students with emotional breakdown experience in ahvaz universities. J Clin Psychol 2016; 8(2): 77–88. doi: 10.22075/ JCP.2017.2238.
13. Lichtlé J, Downes N, Engelberg A wt al. The Effects of parent training programs on the quality of life and stress levels of parents raising a child with autism spectrum disorder: a systematic review of the literature. J Autism Dev Disord 2019; 7(3): 242–262. doi: 10.1007/ s40489-019-00190-x.
14. Watson DC. Self-compassion, the ‘quiet ego’ and materialism. Heliyon 2018; 4(10): e00883. doi: 10.1016/ j.heliyon.2018.e00883.
15. Soheylizad M, Yahaghi Amjad E et al. Relationship between self-esteem, resilience and quality of life in patients with type 2 diabetes in Hamadan in 2015. Pajouhan Sci J 2016; 15(1): 1–8. doi: 10.21859/ psj-15011.
16. Hosseini MA, Dejkam M, Mirlashari J. Correlation between academic achievement and self-esteem in rehabilitation students in Tehran University of Social Welfare & Rehabilitation. Iran J Med Edu 2007; 7(1): 137–142.
17. Fekrat F, Ebrahiminejad G, Razavi NV. The relationship of body image and self-esteem with marital adjustment: a study on female employees of Kerman University of Medical Sciences in 2012–2013. J Health Dev 2015; 3(4): 304–312.
18. Neff KD. The development and validation of a scale to measure self-compassion. Self Ident 2003; 2(3): 223–250. doi: 10.1080/ 15298860390209035.
19. Neff KD, Pisitsungkagarn K, Hsieh YP. Self-compassion and self-construal in the United States, Thailand, and Taiwan. J Cross Cult Psychol 2008; 39(3): 267–285. doi: 10.1177/ 0022022108314544.
20. Iskender M. The relationship between self-compassion, self-efficacy, and control belief about learning in Turkish university students. J Soc Behav Pers 2009; 37(5): 711–720. doi: 10.2224/ sbp.2009.37.5.711.
21. McGehee P, Germer C, Neff K. Core values in mindful self-compassion. Practitioner‘s guide to ethics and mindfulness-based interventions. New York: Springer 2017 : 279–293.
22. Robins RW, Hendin HM, Trzesniewski KH. Measuring global self-esteem: construct validation of a single-item measure and the Rosenberg Self-Esteem Scale. Pers Soc Psychol Bull 2001; 27(2): 151–161. doi: 10.1177/ 014 6167201272002.
23. Pullman H, Allik J. Relations of academic and general self-esteem to school achievement. Person Individ Diff 45(6): 559–564. doi: 10.1016/ j.paid.2008.06.017.
24. Shapurian R, Hojat M, Nayerahmadi H. Psychometric characteristics and dimensionality of a Persian version of Rosenberg Self-esteem Scale. Percept Mot Skills 1987; 65(1): 27–34. doi: 10.2466/ pms.1987.65.1.27.
25. Akin A. Self-compassion and loneliness. Int Online J Educ Sci 2010; 2(3): 702–718.
26. Eller L, Rivero-Mendez M, Voss J et al. Depressive symptoms, self-esteem, HIV symptom management self-efficacy and self-compassion in people living with HIV. AIDS Care 2014; 26(7): 795–803. doi: 10.1080/ 09540121.2013.841842.
27. Joachim G, Acorn S. Stigma of visible and invisible chronic conditions. J Adv Nurs 2000; 32(1): 243–248. doi: 10.1046/ j.1365-2648.2000.01466.x.
28. Arslan C. Anger, self-esteem, and perceived social support in adolescence. J Soc Behav Pers 2009; 37(4): 555–564. doi: 10.2224/ sbp.2009.37.4.555.
29. Harris MA, Orth U. The link between self-esteem and social relationships: a meta-analysis of longitudinal studies. J Pers Soc Psychol 2020; 119(6): 1459–1477. doi: 10.1037/ pspp0000265.
30. Neff K. Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self Ident 2003; 2(2): 85–101. doi: 10.1080/ 15298860390129863.
31. Borji M, Memaryan N, Khorrami Z et al. Spiritual health and resilience among university students: the mediating role of self-esteem. Pastoral Psychol 2020; 69(1): 1–10. doi: 10.1007/ s11089-019-00889-y.
32. Alavian SM, Kachouei H, Moghani LM et al. Marital adjustment in patients with chronic viral hepatitis versus healthy controls. Iran J Psychiatry 2006; 1(4): 153–157.
33. Erol RY, Orth U. Self-esteem and the quality of romantic relationships. Eur Psychol 2017; 21(4): 274–283. doi: 10.1027/1016-9040/a000259.
Labels
Paediatric neurology Neurosurgery NeurologyArticle was published in
Czech and Slovak Neurology and Neurosurgery

2021 Issue 2
Most read in this issue
- Morton’s neuralgia, metatarsalgia
- Moyamoya disease
- Correct and incorrect naming of pictures for the more demanding written Picture Naming and Immediate Recall test (door PICNIR)
- Etiopathogenesis and diagnostics of progressive multifocal leukoencephalopathy in patients treated with natalizumab
