Report of an epicranial arteriovenous malformation
Authors:
C. Castillo-Rangel 1; O. Salinas--Velázquez 2; A. Gomez-Ibarra 1; G. Becerra-Escobedo 3; V. H. Pérez; Pérez 4; G. Marín-Márquez 5
Authors‘ workplace:
Department of Neurosurgery, Clinic of Neurotraumatology, Mexico, Mexico
1; Department of Neurosurgery, Hospital Juarez, Mexico
2; Department of Anesthesiology, Clinic of Neurotraumatology, Mexico, Mexico
3; Neurosurgery Department, Centro Médico Nacional, Siglo XXI, IMSS, Mexico
4; Biophysics Department, Brain Research Institute, Xalapa, Ver., Mexico
5
Published in:
Cesk Slov Neurol N 2021; 84(5): 488-490
Category:
Letters to Editor
doi:
https://doi.org/10.48095/cccsnn2021488
Dear Editor,
Arteriovenous malformation is an abnormal connection between the arterial and venous systems, since the flow regulating the capillary system is absent between them; among these, extracranial malformations that involve the scalp are rare, appearing as pulsatile masses with a propensity to bleed [1].
They are usually present at birth, but show an expansion linked to growth, especially with hormonal increases, where their presence is most evident after adolescence, when their expansion usually compromises local structures and they can even alter the patient’s hemodynamic status.
Multiple treatments may be offered, from surgical resection, tributary ligation, or endovascular treatment.
This malformation was present in a 32-year-old male patient with sporadic smoking and social alcohol drinking with no history of chronic degenerative or pathological diseases relevant to the current clinical condition.
He indicated that, during the last seven years, there was a gradual appearance of a pulsatile mass in the occipital region, which had progressively increased in size until it reached a dimension of 6 x 5 cm (Fig. 1), as well as the appearance of a hyperemic exophytic lesion in the skin, which was prone to profuse bleeding when touched or from rubbing clothes. Other signs or symptoms were denied by the patient, although he was systematically asked about their presence.
Obr. 1. Fotografie před operací.

Physical examination confirmed the presence of a mass measuring approximately 6 x 5 cm with the skin covering this hyperemia, which significantly protruded over the suboccipital region, was soft to the touch, not painful, without adhesion to deep planes transmitting a thrill, and with significant flow sensation with apparent diastolic regurgitation. The rest of the examination data did not suggest any alteration.
From the questioning and exploration, a vascular lesion was suspected and MRI (Fig. 2) revealed data suggesting vascular malformation, and angiography (Fig. 3) confirmed the presence of an epicranial arteriovenous malformation without intracranial communication dependent on afferents of the bilateral occipital branches of the external carotid artery. This lead to the diagnosis of a Schobinger stage III epicranial arteriovenous malformation.
Obr. 2. MR mozku. Absence intenzity odpovídající toku v subokcipitální oblasti.

With the patient’s consent, surgical treatment of the lesion was planned, thus exploration and ligation of the right occipital artery was scheduled (Fig. 4), which was performed with the aid of a neurosurgical microscope without incident. In the postoperative period, a sensation of decreased flow over the lesion was reported by the patient, as well as a depletion of the suboccipital mass without finding the occurrence of ischemic compromise on the skin in the aforementioned area.
One month later, the decision was made to perform contralateral arterial ligation, as well as the resection of the arteriovenous malformation, again with the aid of a neurosurgical microscope where ligation was successfully performed as well as block resection of the arteriovenous malformation after an adipose plane was identified under it. The procedure was completed without incident (Fig. 5), the postsurgical period occurred without incident and recovery of the patient was satisfactory.
Anatomic pathology reported a yellowish-brown (Fig. 6), irregularly ovoid piece measuring 5.0 x 4.6 x 4.0 cm with multiple dilated and congestive blood vessels identifying fibro-fatty tissue with proliferation of venous and arterial cases with irregular walls and congested lumens compatible with arteriovenous malformation.
Prevalence of arteriovenous malformations conveyed in the records of hospitalized patients varies from 1–613 per 100,000 accounting for 1.5% of all vascular lesions, and out of these, approximately 90% of malformations are intracranial [2].
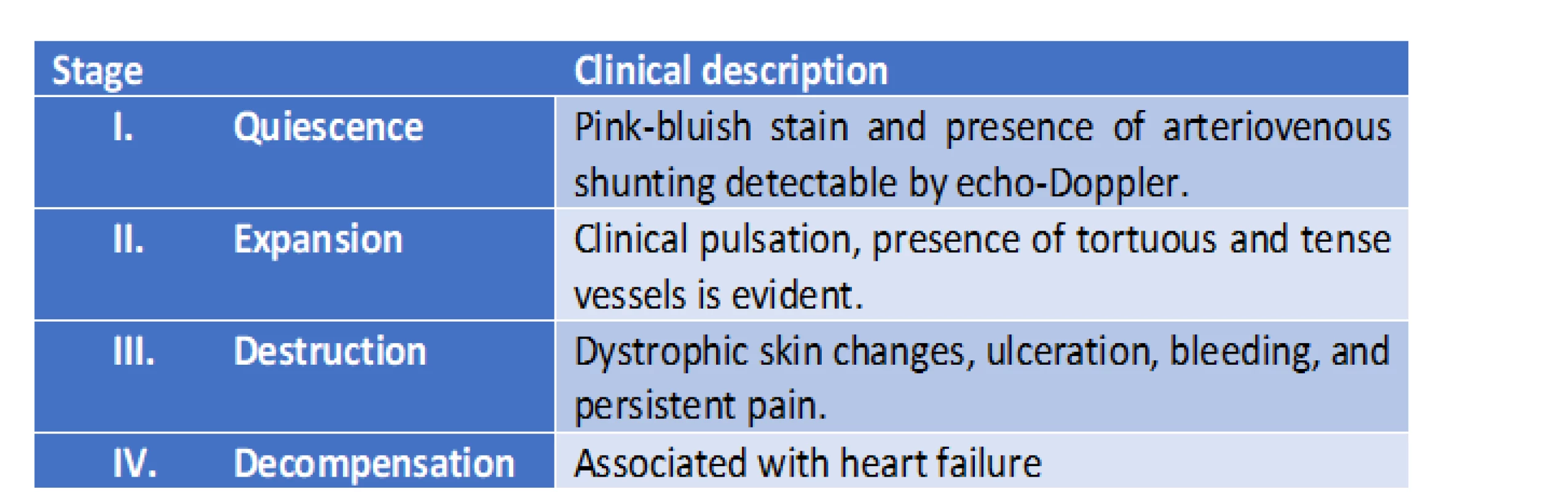
The most widely used classification system is the Schobinger scheme (Tab. 1), which is classified by stages depending on the evolution and progressive characteristics of the malformation. In addition, they may be classified into focal (with a good prognosis and adequate treatment) or diffuse (with a poor prognosis due to the difficulty of treatment and the multiple nutrient vessels) [3].
These lesions are considered congenital errors in vascular development, which occur in early embryonic stages (4–6 weeks of gestation). They are understood as a degeneration failure due to the apoptosis and regression of the arteriovenous channels, creating shunting with circulatory compromise which is initially local. In studies of intracranial arteriovenous malformations, the determining role of endothelial vascular growth factors and platelet-derived growth factors has been identified, although their involvement in the extracranial malformations has not been determined [4].
Upon physical examination, malformations show local erythema and hyperthermia with a prominent pulsating sensation and with an audible murmur and palpable thrill. They tend to have an infiltrative nature (local destruction with deformity and functional compromise) with a risk of bleeding and a high probability of recurrence. Likewise, depending on their development, they can have a strong hemodynamic impact that leads to the decreased capillary oxygenation, ischemia, local hypervascularity, as well as a phenomenon of vascular sequestration with an increased venous pressure. Diagnosis is clinically-based on medical history and clinical examination [5]. On the other hand, super-selective catheterizations help to delineate the nutrient vessels and nidus [6].
Treatment considers the aforementioned points, so there is a wide range of therapeutic possibilities ranging from laser therapy, sclerotherapy, embolization, and surgical resection. Type I and II lesions are considered the easiest to cure, and type III and IV are those with the highest frequency of recurrences and treatment failure [7]. The goal should be focused on complete resection or complete blockage of the nidus, given that partial treatment can induce aggressive growth of the remaining nidus with subsequent worsening of the disease.
Surgical treatment is aimed at complete resection of the nidus, as well as minimizing functional loss and preserving the aesthetics where this modality can be combined with the embolization after angiography with the intention of reducing the bleeding [8], but a meticulous technique with the use of bipolar cautery and gel foam can adequately control intraoperative bleeding. With the appropriate use of flaps, it can even stabilize the hemodynamic status of the area where the malformation is resected [9].
Finally, neurosurgery was decided in 2 stages due to safeguarding the irrigation of the skin, and 100% resection of the malformation avoiding any recurrence, a very adequate result.
The Editorial Board declares that the manu script met the ICMJE “uniform requirements” for biomedical papers.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Gerardo Marín Márquez, MD
Dr. Castelazo Ayala s/n
Industrial Animas
91190 Xalapa-Enríquez
Mexico
e-mail:
drmarin.neuroscience@gmail.com
Accepted for review: 8. 5. 2021
Accepted for print: 21. 6. 2021
An extended version of the article is available at csnn.eu.
Sources
1. Hanuška J, Klener J. Significant brain oedema in unruptured brain arteriovenous malformation – a case report. Cesk Slov Neurol N 2017; 80/113 (3): 350–352. doi: 10.14735/amcsnn2017350.
2. Eivazi B, Werner JA. Management of vascular malformations and hemangiomas of the head and neck – an update. Curr Opin Otolaryngol Head Neck Surg 2013; 21 (2): 157–163. doi: 10.1097/MOO.0b013e32835e15a9.
3. Zou Y, Quiao C, Xiaoxi L et al. Clinical course of extracranial arteriovenous malformations. J Craniofac Surg 2020; 31 (2): 372–376. doi: 10.1097/SCS.0000000000006 018.
4. Couto JA, Huang AY, Konczyk DJ et al. Somatic MAP2K1 mutations are associated with extracranial arteriovenous malformation. Am J Hum Genet 2017; 100 (3): 546–554. doi: 10.1016/j.ajhg.2017.01.018.
5. Kim JB, Lee JW, Choi KY et al. Clinical characteristics of arteriovenous malformations of the head and neck. Dermatol Surg 2017; 43 (4): 526–533. doi: 10.1097/DSS. 0000000000000993.
6. Vaišnytė B, Vajauskas D, Palionis D et al. Diagnostic methods, treatment modalities, and follow-up of extracranial arteriovenous malformations. Medicina (Kaunas) 2012; 48 (8): 388–398.
7. Cho SK, Do YS, Shin SW et al. Arteriovenous malformations of the body and extremities: analysis of therapeutic outcomes and approaches according to a modified angiographic classification. J Endovasc Ther 2006; 13 (4): 527–538. doi: 10.1583/05-1769.1.
8. Richter GT, Friedman AB. Hemangiomas and vascular malformations: current theory and management. Int J Pediatr 2012; 645–678. doi: 10.1155/2012/645 678.
9. Kansy K, Bodem J, Engel M et al. Interdisciplinary treatment algorithm for facial high-flow arteriovenous malformations, and review of the literature. J Craniomaxillofac Surg 2018; 46 (5): 765–772. doi: 10.1016/ j.jcms.2018.03.002.
Labels
Paediatric neurology Neurosurgery NeurologyArticle was published in
Czech and Slovak Neurology and Neurosurgery

2021 Issue 5
Most read in this issue
- Analgesic-muscle relaxant infusion in back pain therapy – technological and clinical aspects
- Ofatumumab – a new high-efficacy treatment for relapsing forms of multiple sclerosis
- Ultrasound-guided sacroiliac joint injection
- A syndrome of progressive ataxia and palatal tremor in a patient with mild bilateral idiopathic hypertrophic olivary degeneration