Underuse of Oral Anticoagulation in Primary Prevention of Cardioembolic Stroke – Results of a Descriptive Prevalence Study
Nedostatečná antikoagulační terapie v primární prevenci kardioembolických cévních mozkových příhod – výsledky deskriptivní prevalenční studie
Úvod:
Perorální antikoagulační terapie (OAT) je účinnou léčbou užívanou při prevenci kardioembolických cévních mozkových příhod (CMP). Cílem studie bylo zhodnotit výskyt kardioembolických CMP, zejména způsobených fibrilací síní (FS) a užívání OAT u pacientů s akutní ischemickou CMP a FS, včetně porovnání trendů v rámci pětiletého období.
Metodika:
V nemocniční deskriptivní prevalenční studii byla analyzována data všech konsekutivních pacientů hospitalizovaných s jejich první ischemickou CMP v letech 2007, 2008 a 2012. U pacientů s kardioembolickou CMP byl zaznamenán výskyt FS (jak již známé, tak nově zjištěné), její léčba a přítomnost kontraindikací užívání OAT v případě dříve známé FS.
Výsledky:
Mezi pacienty hospitalizovanými v letech 2007 (n = 293), 2008 (n = 299) a 2012 (n = 307) byla přítomna kardioembolická CMP u 34,1%; 39,1% a 37,1% pacientů, FS se vyskytla u 75,0%; 76,9% a 95,0% pacientů s kardioembolickou CMP, přičemž FS byla známá před ischemickou CMP u 46,0%; 53,8% a 61,0% pacientů s kardioembolickou CMP. OAT nebyla nasazena před ischemickou CMP u 80,4%; 79,4% a 77,0% pacientů se známou FS, ačkoli její podání bylo kontraindikováno u pouze u 45,9%; 50,0% a 38,3% z těchto pacientů (p > 0,05 ve všech případech).
Závěr:
Výsledky této studie prokázaly významné procento nedostatečně léčených pacientů s kardioembolickou CMP a známou FS v rámci primární prevence CMP, přičemž v posledních pěti letech není přítomen významný trend ke zlepšení.
Klíčová slova:
antikoagulační terapie – antiagregační terapie – fibrilace síní – kardioembolická cévní mozková příhoda – prevence ischemické cévní mozkové příhody
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Authors:
M. Král 1; R. Herzig 1; D. Sanak 1; D. Skoloudik 1; A. Bártková 1; T. Veverka 1; R. Obereignerů 1; M. Kovacik 2; J. Zapletalová 3
Authors‘ workplace:
Comprehensive Stroke Center, Department of Neurology, Faculty of Medicine and Dentistry, Palacky University and University Hospital, Czech Republic
1; Department of Neurology, Central Military Hospital, Ružomberok, Slovakia
2; Department of Medical Biophysics, Faculty of Medicine and Dentistry, Institute of Molecular and Translational Medicine, Palacky University, Czech Republic
3
Published in:
Cesk Slov Neurol N 2014; 77/110(1): 59-63
Category:
Original Paper
Overview
Background:
Oral anticoagulation therapy (OAT) is an effective treatment used in the prevention of cardioembolic stroke (CS). The aim was to assess the incidence of CS, especially caused by atrial fibrillation (AF), to analyse the OAT administration in patients with AF and acute ischemic stroke (AIS), and to investigate trends in AOT administration over a 5‑year period.
Methods:
In a hospital‑based, descriptive prevalence study, data on all first‑ time AIS patients admitted in 2007, 2008 and 2012 were analyzed. In CS patients, the incidence of AF (both in the medical history and recently), its treatment and the presence of contraindications to OAT administration in the case of previously known AF were recorded.
Results:
The incidence of CS and AF among the 2007 (n = 293), 2008 (n = 299) and 2012 (n = 307) patients was as follows: 34.1, 39.1 and 37.1% had CS; 75.0, 76.9 and 95.0% of CS patients had AF; 46.0, 53.8 and 61.0% of CS patients were diagnosed with AF prior to AIS. OAT was not used in 80.4, 79.4 and 77.0% of patients with AF known prior to AIS (although its administration was contraindicated in only 45.9, 50.0 and 38.3% of these patients, respectiverly) (p > 0.05 in all cases).
Conclusions:
The results of the present study demonstrated major undertreatment with OAT in the prevention of CS in patients with previously known AF with no trend towards improvement during the last five years.
Key words:
anticoagulation – antiplatelet therapy – atrial fibrillation – cardioembolic stroke – stroke prevention
Background
Stroke is one of the leading causes of morbidity, mortality and long‑term disability worldwide [1]. It is also the second most common cause of dementia, the most frequent cause of epilepsy in the elderly, and a frequent cause of depression [2– 3]. In the USA, ≈ 795,000 incident strokes occur each year. In 2010, this resulted in one out of 17 deaths with an estimated direct and indirect cost of 73.7 billion USD [4]. A very similar situation has been noted in other “developed” countries. The incidence rates in the European Union (EU) varied between 2.0 and 2.5 per 1,000 inhabitants in the western part and between 3.0 and 5.0 per 1,000 inhabitants in the eastern part [5]. Ischemic stroke (IS) represents the most common type of stroke worldwide, accounting for 87% of strokes in the USA and 58– 70% in the EU [5].
Cardio‑ embolization (CE) together with atherosclerosis and small‑vessel disease are the most common causes of IS. Various heart diseases may cause embolization from the heart to the cerebral arteries (e. g. aneurysm of the left atrium and ventricle, sick sinus syndrome, mitral stenoses, heart myxoma, heart thrombus or myocardial infarction). However, the most frequent CE‑based cause is atrial fibrillation (AF). The global prevalence of cardioembolic stroke (CS) is considered to be ≥ 20% of all IS cases [6– 7]. Moreover, ≈ 30% of idiopathic IS may be due to CS. Thus, the prevalence of CS may increase, reaching ≤ 50% [8].
AF is a strong independent risk factor for IS. Its prevalence is 4– 5% in the 60– 75 years age group and ≤ 10% in older population [9– 10]. Studies have shown that the incidence of AF is increasing not only due to aging population but also in particular age categories during the last 50 years [11– 12]. In patients with AF, movement of emboli into the central nervous system (CNS) represents ≈ 80% of thrombembolisms. AF is an independent risk factor for IS and, therefore, for increased mortality and morbidity in thrombembolic disease for all types of AF [13– 14].
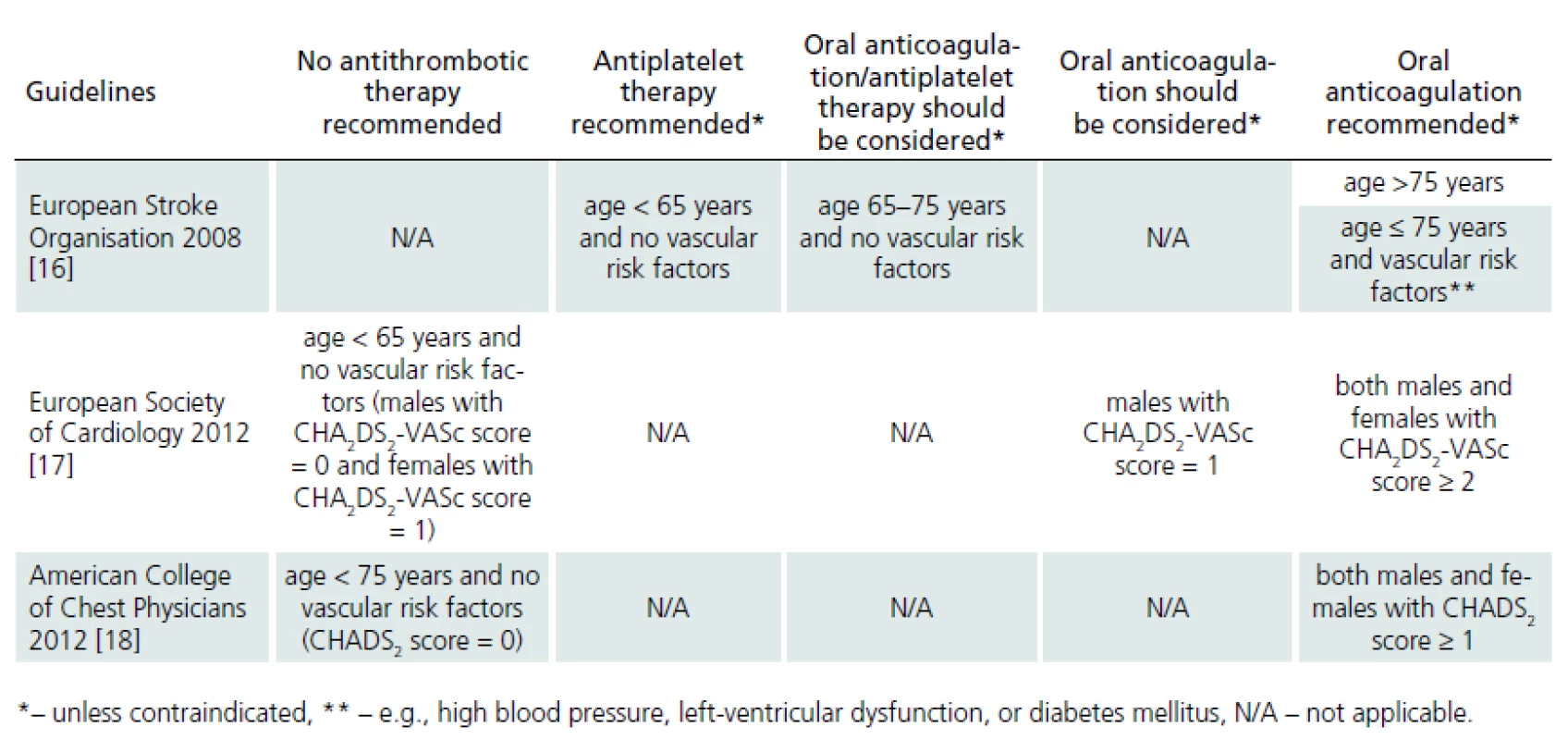
CS requires a different strategy for secondary preventive treatment when compared with atherothrombotic IS. Anticoagulant therapy is associated with 68% reduction in the relative risk of subsequent IS, whereas antiplatelet therapy reduced the risk of IS by ≈ 20% [15]. Indications for antithrombotic therapy (oral anticoagulation or antiplatelet therapy) in patients with non‑valvular AF according to the valid international guidelies [16– 18] are presented in Tab. 1.
The aim of the present study was to assess:
- the incidence of CS (in particular that caused by chronic or paroxysmal AF) and
- OAT administration as the primary prevention in patients with AF and acute ischemic stroke (AIS), and to investigate the time trend during a 5‑year period.
Methods
In this hospital‑based, descriptive study, data of all first‑ ever AIS patients admitted to the Department of Neurology, University Hospital Olomouc (serving the Moravia region in the Czech Republic with 130,000 inhabitants) in 2007, 2008 and 2012 were gathered and analyzed. The cohort involved patients treated by general practitioners as well as hospital outpatients. Data were collected from medical records and/ or medical information systems. AIS etiology was evaluated as being “cardioembolic”, “atherothrombotic”, “small‑vessel disease” or “other” using the ASCO criteria [19].
In CS patients, occurrence of AF (in medical history and recently) and of other cardioembolic sources and their treatment were recorded. The diagnosis of a new AF was based on ECG examination performed at admission and on subsequent bed‑ side (at least 24- hour) ECG monitoring at the stroke unit and ECG Holter monitoring in patients with no previous evidence of AF. A history of previous diagnoses (arterial hypertension, myocardial infarction, ischemic heart disease, peripheral arterial disease, DM) and concomitant therapy (antihypertensives, antidiabetics, hypolipidemics) was recorded. Stroke‑ prevention therapy (antiplatelets, OAT, none) before and at AIS onset were also recorded. Indications and contraindications to OAT administration were evaluated in patients without OAT and in those with prior AF as ascertained from medical records. OAT contraindications included: previous systemic bleeding; predisposition to gastrointestinal bleeding or to bleeding into the urinary tract, recent intracranial hemorrhage or predisposition to intracranial bleeding, severe hepatic insufficiency or cirrhosis, untreated or uncontrolled arterial hypertension, history of frequent falls due to neurological or other medical conditions, brain or eye surgery, infectious endocarditis or bleeding into the pericardium, and lack of patient cooperation (e. g. due to dementia, psychosis, or alcohol abuse).
Data were analysed using SPSS 15.0 (SPSS, Chicago, IL, USA). Categorical variables were compared using the Pearson chi‑ squared test or Fisher’s exact test. The Mann‑Whitney U‑ test was used to compare continuous variables. The normality of distribution was tested using the Kolmogorov‑ Smirnov test. P < 0.05 was considered significant. Additional analyses were performed for selected categorical variables with the percentual Z test (significance level p = 0.05 if Z value > 1.96) and for continuous variables with the Student’s t‑test. We used the analytical and statistical tools in Microsoft© Office Excel 2007. Data were analysed at the Department of Medical Biophysics, Palacky University (Olomouc, Czech Republic).
Results
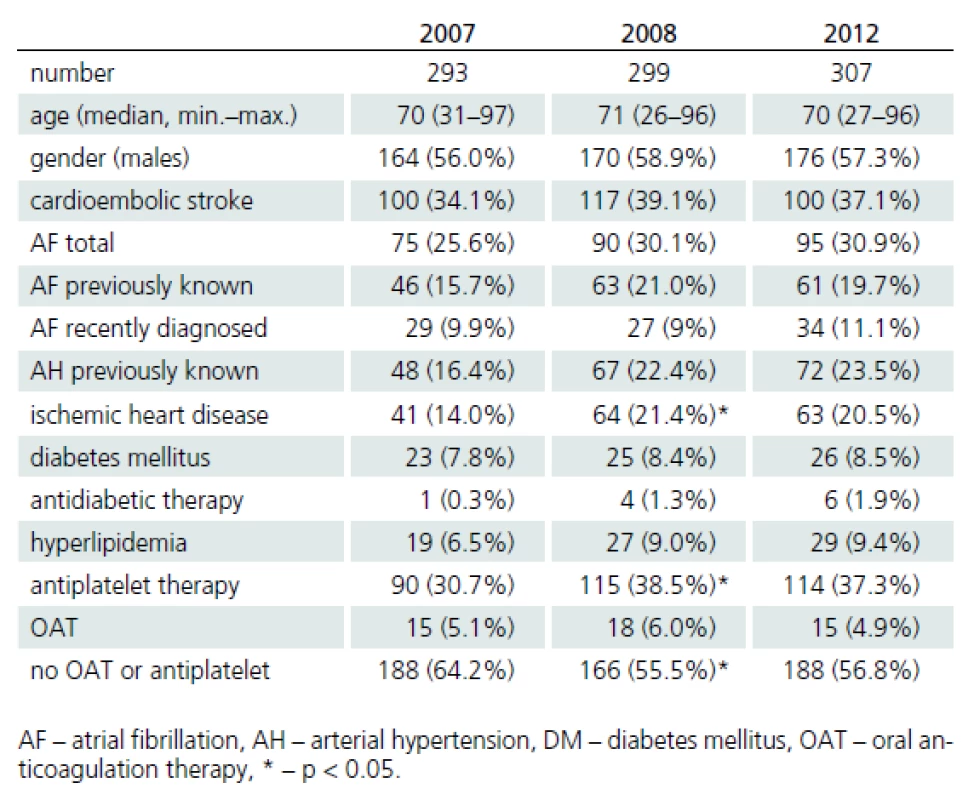
The study group consisted of 899 AIS patients admitted in 2007, 2008 and 2012. Patient demographic and epidemilogical characteristics by the three admission years (including the comparison of the time trends) are presented in Tab. 2. No significant differences were found between the observed parameters of AIS patients admitted in the respective years (p > 0.05 in all cases).
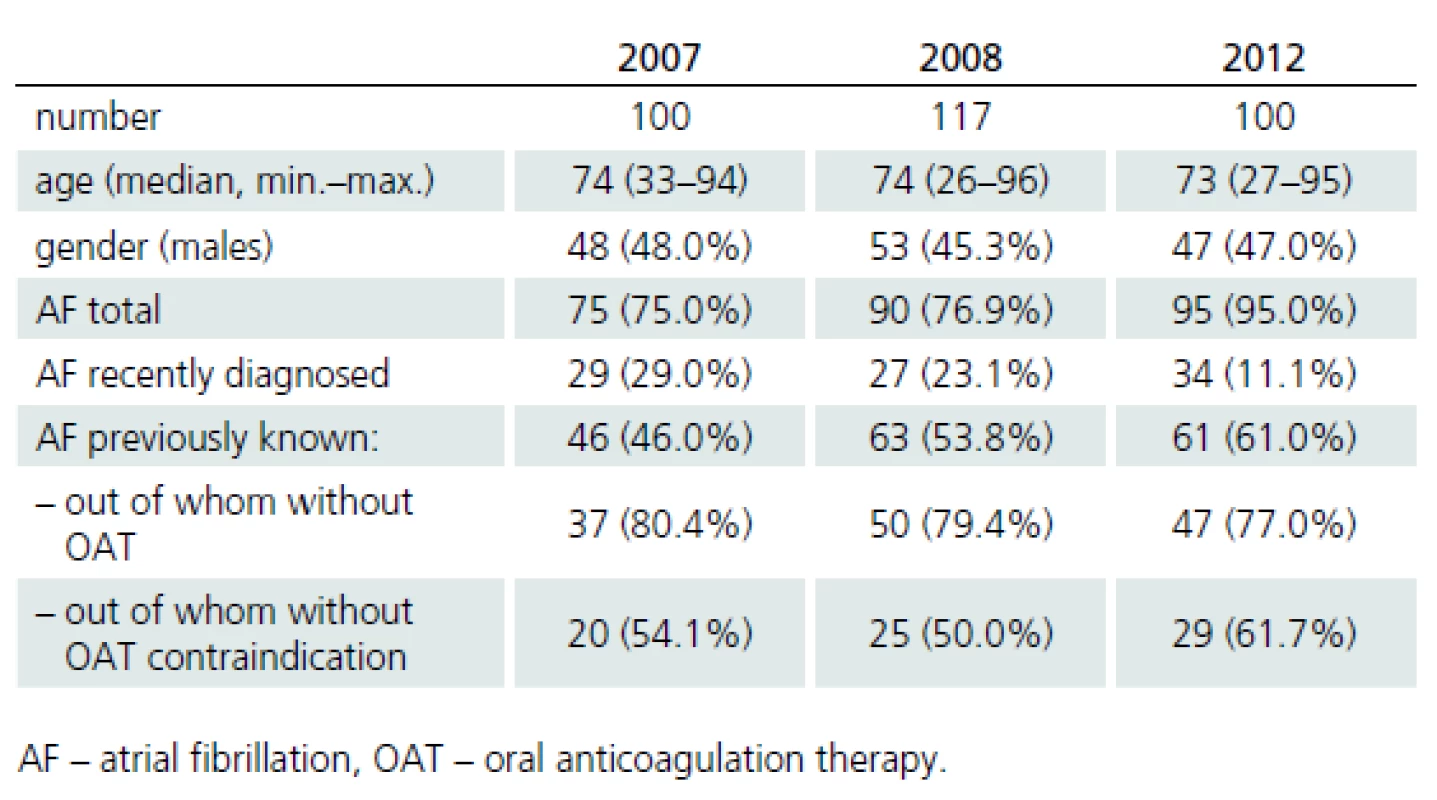
In 2007, 2008 and 2012, cardioembolic etiology of AIS was diagnosed in 34.1, 39.1 and 37.1%, of patients, respectively; AF was present in 75.0, 76.9 and 95.0% of cases, respectively; and 46.0, 53.8 and 61.0% of CS patients, respectively, had known AF before stroke. No significant differences were found in the demographic characteristics of patients with CS between 2007, 2008 and 2012 (p > 0.05 in all cases) (Tab. 2). OAT was not used in the majority of CS patients with known AF before stroke (80.4, 79.4 and 77.0% of patients), although its administration was contraindicated in 45.9, 50.0 and 38.3% of these patients in each respective year (Tab. 3).
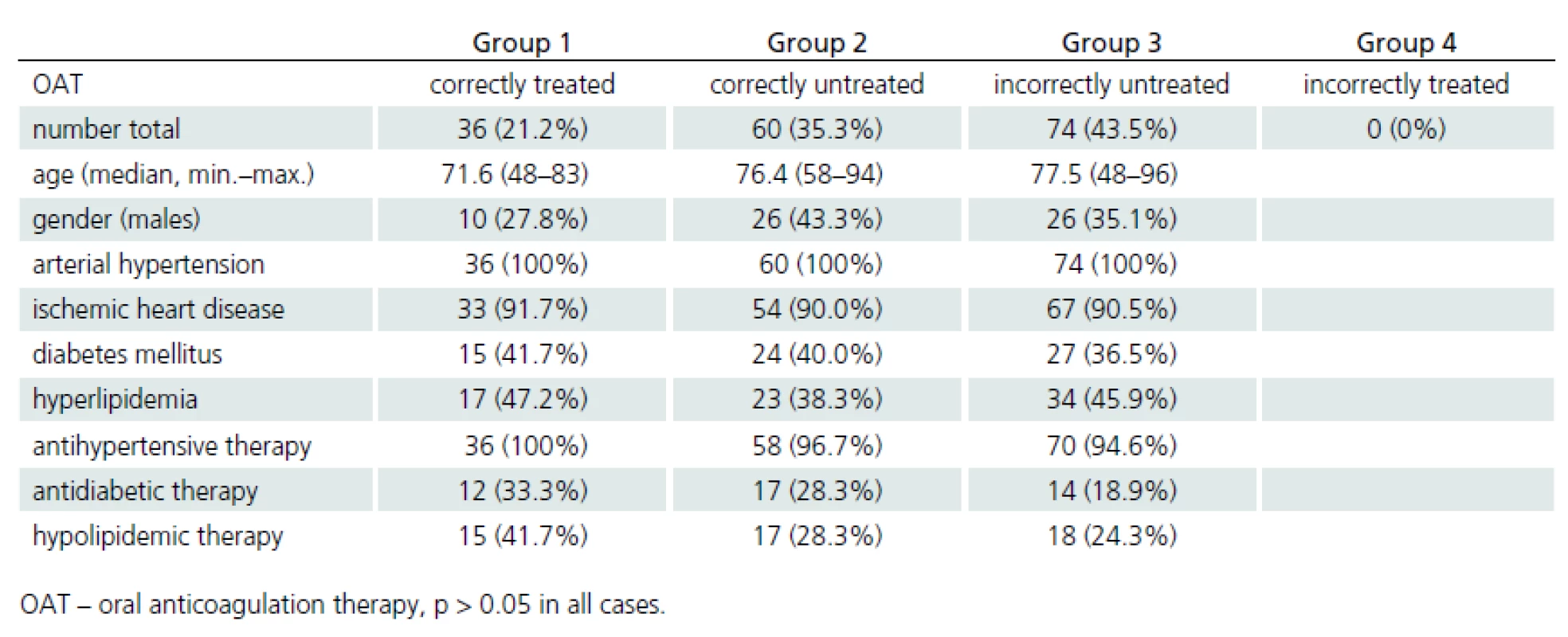
Patients with known AF before CS were classified as:
- a) correctly treated (OAT administration in a patient without contraindication; group 1),
- b) correctly untreated (no OAT administration in the presence of OAT contraindication; group 2),
- c) incorrectly untreated (no OAT administration and no OAT contraindication; group 3),
- d) incorrectly treated (OAT administration in a patient with contraindication; group 4).
Characteritics of patients in each group are presented in Tab. 4. Only 56.5% of patients were correctly treated with OAT (21.2%, group 1) or untreated (35.3%, group 2), whereas 43.5% were incorrectly untreated (group 3). No patients were incorrectly treated with OAT (group 4). No significant changes were observed in the proportion of patients in each subgroup between the respective years (2007, 2008 and 2012). No significant differences were found in the observed parameters between subgroups (p > 0.05 in all cases).
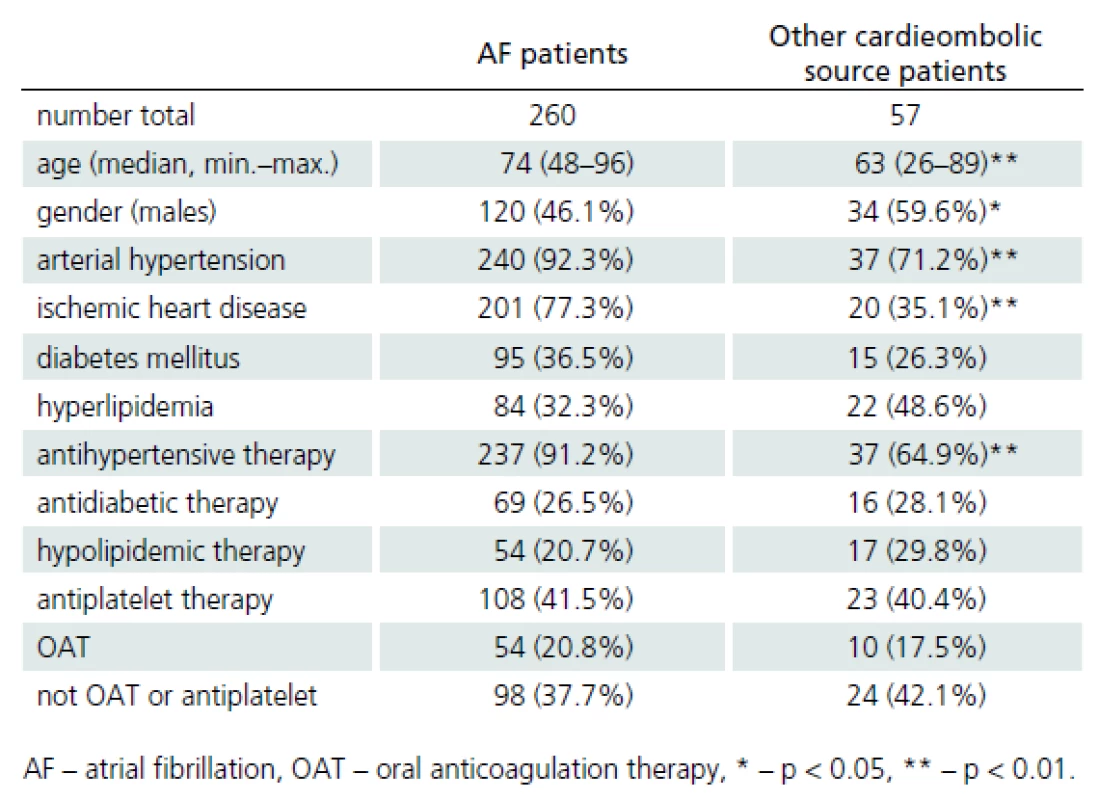
Comparison of CS patients with AF (both in medical history and recently diagnosed) and with other sources of cardioembolism is presented in Tab. 5. AF patients were significantly older. Female gender, arterial hypertension (including antihypertensive treatment) and ischemic heart disease were significantly more frequent in AF patients.
Conclusions
In the present study, 43.5% of patients with AF known before CS and who had no contraindication to OAT were incorrectly untreated with OAT. This confirms the lack of primary IS prevention in this high‑risk AF group. Interestingly, the proportion of AF patients appropriately treated with OAT in the present study was not lower than that in the general population [20]. The contrary could be expected since the risk of IS is higher in incorrectly untreated AF patients. The use of OAT was not statistically different between AF patients and CS patients with other cardioembolic sources.
Moreover, a general tendency to undertreatment of other previously known vascular risk factors (e. g. arterial hypertension, DM, hyperlipidemia) was found in this subgroup of patients incorrectly untreated with OAT, whereas the situation was much better in the subgroup of patients correctly treated with OAT.
Higher age in these patients compared to correctly OAT treated AF patients (median, 73.5 vs. 71.7 years) could explain this finding (even though this difference was not significant). Conversely, a significantly higher age was found in AF patients correctly untreated with OAT compared to patients correctly treated with OAT (median, 78.3 vs. 71.7 years). This is consistent with age‑related increase in the incidence of OAT contraindications. Nevertheless, age alone does not represent a contraindication to OAT use. No significant differences were found in previously known vascular risk factors and diagnoses (i.e., arterial hypertension, ischemic heart disease, DM, peripheral arterial disease, hyperlipidemia) and administration of antihypertensive, antidiabetic and hypolipidemic drugs between the subgroups of patients with known AF prior to CS. For example, all these patients had arterial hypertension and 38.8% were known to have DM. The prevalence of both these risk factors was notably higher than the prevalence of arterial hypertension (52.4%) and DM (15.1%) reported by Herman et al. in patients with stroke of various etiologies within a Dutch community [21].
Therefore, possible patient non‑compliance may not be the main reason for the absence of OAT in the primary prevention in AF patients. One may hypothesize that some of the physicians caring for AF patients neglected or underestimated the risks of AF (as well as the role of other vascular risk factors) or overestimated the possible risks of OAT.
Several limitations of the present study should be mentioned. Firstly, the cohort represented consecutive patients with acute IS and AF admitted to the Department of Neurology only, and some patients admitted primarily to the Department of Internal Medicine (due to a predominant risk of internal injury) may have been missed. However, the number of such patients is expected to be quite small and thus with no influence on the statistical analysis. Secondly, referring physicians were not asked about the exact reason for not prescribing antithrombotic (antiplatelet and OAT) treatment to their patients. Moreover, the analyzed set of patients hospitalized due to stroke represents only a small proportion of all patients, who should, for various reasons, be prescribed OAT as the primary prevention.
In conclusion, the results of the present study demonstrated major undertreatment with OAT in the prevention of CS in patients with previously known AF, without any trend to improvement during the last 5 years. Therefore, recently published guidelines should be actively disseminated among physicians caring for AF patients to ensure that patients are provided with the appropriate therapy and to lower the risk of CS.
The study was partially supported by the Internal Grant Agency, Ministry of Health, Czech Republic grants number NT/ 11386–6/2010, NT/11046–6/2010 and NT14288-3/2013 and by the conceptual development of research organization (FNOl, 00098892).
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Accepted for review: 2. 5. 2013
Accepted for print: 3. 10. 2013
MUDr. Michal Kral, MD
Department of Neurology
Palacky University Medical School
I. P. Pavlova 6
775 20 Olomouc
e-mail: kral_michal@centrum.cz
Sources
1. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006; 367(9524): 1747– 1757.
2. Rothwell PM, Coull AJ, Silver LE, Fairhead JF, Giles MF, Lovelock CE et al. Population‑based study of event‑ rate, incidence, case fatality, and mortality for all acute vascular events in all arterial territories (Oxford Vascular Study). Lancet 2005; 366(9499): 1773– 1783.
3. O’Brien JT, Erkinjuntti T, Reisberg B, Roman G, Sawada T, Pantoni L et al. Vascular cognitive impairment. Lancet Neurol 2003; 2(2): 89– 98.
4. Lloyd‑ Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive summary: Heart disease and stroke statistics – 2010 update: a report from the American Heart Association. Circulation 2010; 121(7): 948– 954.
5. Brainin M, Bornstein N, Boysen G, Demarin V. Acute neurological stroke care in Europe: results of the European Stroke Care Inventory. Eur J Neurol 2000; 7(1): 5– 10.
6. Albers GW, Amarenco P, Easton JD, Sacco RL, Teal P.Antithrombotic and thrombolytic therapy for ischemic stroke: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126 (3 Suppl): 483S‑ 512S.
7. Kistler JP. Cerebral embolism. Compr Ther 1996; 22(8): 515– 530.
8. Sacco RL, Ellenberq JH, Mohr JP, Tatemichi TK, Hier DB,Price TR et al. Infarcts of undetermined cause: the NINCDS Stroke Data Bank. Ann Neurol 1989; 25(4): 382– 390.
9. Lévy S, Breithardt G, Campbell RW, Camm AJ, Daubert JC, Allessie M et al. Atrial fibrillation: current knowledge and recommendations for management. Working Group on Arrhythmias of the European Society of Cardiology. Eur Heart J 1998; 19(9): 1294– 1320.
10. Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA et al; American College of Cardiology; American Heart Association Task Force; European Society of Cardiology Committee for Practice Guidelines; European Heart Rhythm Association; Heart Rhythm Society. ACC/ AHA/ ESC 2006 guidelines for the management of patients with atrial fibrillation: full text. A report of the American College of Cardiology/ American Heart Association Task Force on practice guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation) developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Europace 2006; 8(9): 651– 745.
11. Pedersen OD, Brendrop B, Køber L, Torp‑ Pedersen C.Prevalence, prognostic significance and treatment of atrial fibrillation in congestive heart failure with particular reference to the DIAMOND‑ CHF study. Congest Heart Fail 2003; 9(6): 333– 340.
12. Lip GYH, Godfredsen J. Cardiac arrhythmias a clinical approach. 1st ed. Edinburgh: Mosby 2003.
13. Krahn AD, Manfreda J, Tate RB, Mathewson FA, Cuddy TE. The natural history of atrial fibrillation: incidence, risk factors and prognosis in the Manitoba Follow‑up Study. Am J Med 1995; 98(5): 476– 484.
14. Lake FR, Cullen KJ, deKlerk NH, McCall MG, Rosman DL. Atrial fibrillation and mortality in an elderly population. Aust N Z J Med 1989; 19(4): 321– 326.
15. Hart RG, Benavente O, McBride R, Pearce LA. Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta‑analysis. Ann Intern Med 1999; 131(7): 492– 501.
16. European Stroke Organisation (ESO) Executive Committee; ESO Writing Committee. Guidelines for Management of Ischaemic Stroke and Transient Ischaemic Attack 2008. Cerebrovasc Dis 2008; 25(5): 457– 507.
17.Camm AJ, Lip GYH, De Caterina R, Savelieva I, Atar D, Hohnloser SH et al. An update of the 2010 ESC Guidelines for the management of atrial fibrillation. Eur Heart J 2012; 33(21): 2719– 2747.
18. Guyatt GH, Akl EA, Crowther M, Gutterman DD, Schünemann HJ; American College of Chest Physicians Antithrombotic Therapy and Prevention of Thrombosis Panel. Executive summary: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence‑ Based Clinical Practice Guidelines. Chest 2012; 141 (Suppl 2):7S‑ 47S.
19. Amarenco P, Bogousslavsky J, Caplan LR, Dohnán GA, Hennerici MG. New Approach to Stroke Subtyping: The A‑ S‑ C‑ O (Phenotypic) Classification of Stroke. Cerebrovasc Dis 2009; 27(5): 502– 508.
20. Nieuwlaat R, Capucci A, Lip GY, Olsson SB, Prins MH, Nieman FH et al. Euro Heart Survey Investigators: Antithrombotic treatment in real‑life atrial fibrillation patients: a report from the Euro Heart Survey on Atrial Fibrillation. Eur Heart J 2006; 27(24): 3018– 3026.
21. Herman B, Leyten AC, van Luijk JH, Frenken CW, Op de Coul AA, Schulte BP. An evaluation of risk factors for stroke in a Dutch community. Stroke 1982; 13(3): 334– 339.
Labels
Paediatric neurology Neurosurgery NeurologyArticle was published in
Czech and Slovak Neurology and Neurosurgery

2014 Issue 1
Most read in this issue
- Microsurgical Resection of Symptomatic Pineal Cysts
- Surgical Treatment of Hydrocephalus
- Stiff‑ person Syndrome Associated with Myotonic Dystrophy Type 2 – a Case Report
- International Standards for Neurological Classification of Spinal Cord Injury – Revision 2013
