Moyamoya syndrome associated with polycystic kidney disease – a rare case report and literature review
Authors:
D. Kefang 1,2; Z. Shaosen 1; W. Rong 1; Z. Yan 1; Z. Dong 1
Authors place of work:
Department of Neurosurgery, Beijing, Tiantan Hospital, Capital Medical University, China National Clinical Research, Center for Neurological Diseases, Beijing, China
1; Xingtai Third Hospital, Xingtai, Hebei, China
2
Published in the journal:
Cesk Slov Neurol N 2020; 83/116(4): 428-430
Category:
Dopis redakci
doi:
https://doi.org/10.14735/amcsnn2020428
Dear editorial office,
Moyamoya disease is a chronic cerebrovascular disorder which is characterized by progressive stenoses and/or occlusions of the intracranial internal carotid artery (ICA) and its proximal branches, involving the development of a basal collateral network [1]. Conditions such as atherosclerosis, polycystic kidney disease (PKD), neurofibromatosis, or meningitis have been well recognized to be associated with moyamoya syndrome [2]. PKD is characterized by the presence of bilateral renal cysts and is always associated with vascular abnormalities including intracranial aneurysms, dilatation of the aortic root, and dissection of the thoracic aorta [3]. We herein report a rare case of moyamoya syndrome associated with PKD.
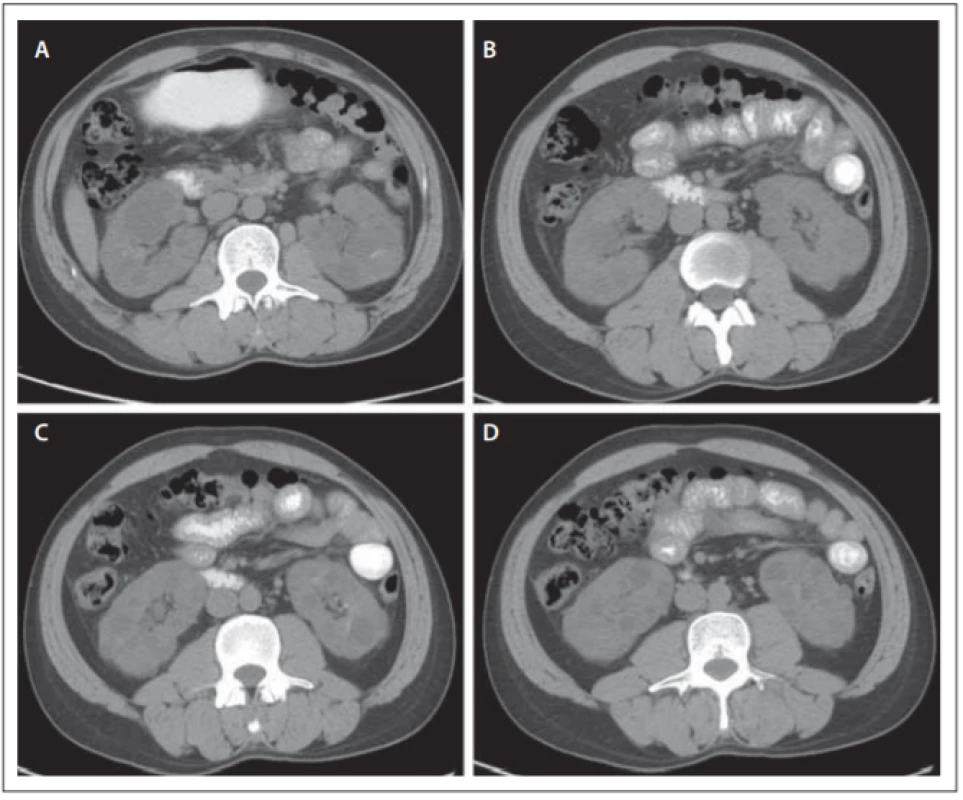
A 34-year-old male patient suddenly suffered from an intensive headache 2 months ago and lost consciousness 2 days later. CT revealed intraventricular hemorrhage. The headache reocurred 1 month after the first episode and CT revealed intraventricular hemorrhage again. Digital subtraction angiography revealed typical bilateral findings of moyamoya disease with extensive cortical brain collateralization (Fig 1). The abdominal CT scan showed the presence of bilateral multiple renal cysts (Fig 2). The patient was treated with combined revascularization surgery (superficial temporal artery-middle cerebral artery anastomosis and encephalo-duro-arterio-synangiosis) without neurologic deterioration. His father, older sister, and older brother were also diagnosed with PKD.
Obr. 1. DSA karotid v předozadním zobrazení. Oboustranná okluze distálních segmentů
vnitřních karotid s cévněním typu moyamoya u baze lební (A, B).
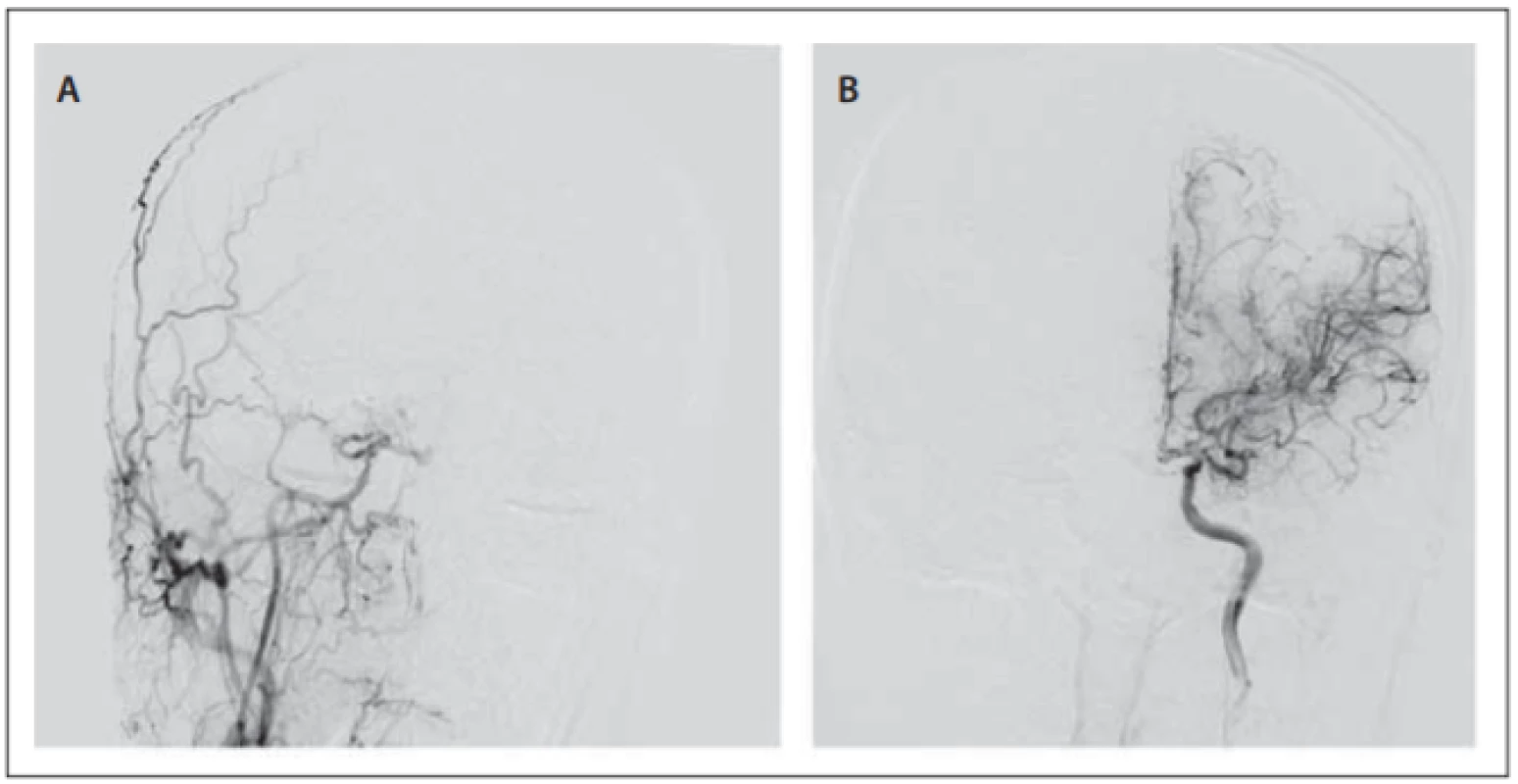
Obr. 1 – pokračování. Předozadní zobrazení
vnějších karotid na obou stranách svědčící
pro částečnou kompenzaci krevního zásobení mozku levou vnější karotidou
(C, D). Angiogramy vertebrálních tepen prokázaly, že vertebrální tepny na obou stranách částečně kompenzovaly krevní zásobení mozku.

Obr. 2. CT snímky břišní dutiny. Polycystóza ledvin oboustranně.
In moyamoya syndrome, vessel stenosis or occlusion is accompanied by an abnormal vascular network associated with an underlying disease [4]. The annual incidence of moyamoya syndrome is 0.11/100,000, and its prevalence is 4/100,000 [5]. Underlying diseases include atherosclerosis (29%), Down syndrome (15.1%), von Recklinghausen disease (14%), brain tumor or brain irradiation (7.5%), autoimmune disease (7.5%), and hyperthyroidism (7.5%) [6]. PKD is characterized by bilateral renal cysts and other abnormalities, including vascular disease. Vascular manifestations include intracranial and other arterial aneurysms and, more rarely, dolichoectasia, dilation of the aortic root, dissection of the thoracic aorta, and, possibly, coronary artery aneurysms [7]. PKD is also known as one of the underlying diseases of moyamoya syndrome which was rarely reported. Only 2 cases of moyamoya syndrome associated with PKD have been reported in the literature. In 1988, Pracyk et al reported the first case of a female patient whose arteriogram showed bilateral occlusion of the ICAs with “puff of smoke” collateralization arising from the circle of Willis. She was also diagnosed with arterial hypertension and eosinophilic granuloma. The patient finally died of the right putaminal hemorrhage with extension into the ventricle [8]. The second case was reported in 2012. The patient was diagnosed with moyamoya syndrome with PKD. Neurologic examination showed choreoathetosis in the right side of the body. Her twin sister was diagnosed with moyamoya syndrome with an intestinal duplication cyst [9]. Generally, moyamoya disease presents with 2 main types of symptoms: ischemia and hemorrhage [2]. For hemorrhagic moyamoya disease, a cause of hemorrhage may be cerebral aneurysms [10]. PKD confers the highest risk of intracranial berry aneurysm. Pracyk et al believed that rupture of an aneurysm could account for the cerebral hemorrhage found in their patient [8]. Our case included intraventricular hemorrhage which may also be due to a microaneurysm rupture. Only 1 case included choreoathetosis which may be due to ischemia. This may indicate that patients with moyamoya syndrome associated with PKD were prone to cerebral hemorrhage.
The prevalence of moyamoya disease has an ethnic bias, with a high incidence of the disease in Eastern Asian countries such as Japan, Korea and China. And this is the first report of an Asian person with PKD associated with moyamoya syndrome.
Disclosures
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manu script met the ICMJE “uniform requirements” for biomedical papers.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Accepted for review: 24. 12. 2019
Accepted for print: 29. 4. 2020
Dong Zhang
Department of Neurosurgery Beijing Tiantan Hospital Capital Medical University,
No. 119 South Fourth Ring West Road
Fengtai District
Beijing 100070
China
e-mail: zhangdongtgy@163.com
Štítky
Dětská neurologie Neurochirurgie NeurologieČlánek vyšel v časopise
Česká a slovenská neurologie a neurochirurgie

2020 Číslo 4
Nejčtenější v tomto čísle
- It is evident when to make a surgery for lumbar disc herniation?
- CGRP monoclonal antibodies in the treatment of migraine – indication criteria and therapeutic recommendations for the Czech Republic
- Current diagnostics of secondary progressive form of multiple sclerosis and its treatment with siponimod
- Cytotoxic lesions of the corpus callosum (CLOCCs)
