A Dorsal Neurenteric Cyst of the Craniocervical Junction – a Case Report
Neurenterická cysta kraniocervikální junkce – kazuistika
Neurenterická cysta (NEC) je velmi vzácná diagnóza. Tato vrozená vada je definována jako cysta, která je vystlána mucin secernujícím epitelem, obdobný tomu, který se vyskytuje v gastrointestinálním traktu. Neurenterická cysta se může vytvořit kdekoli podél neurální osy, ale predominantě ve spodních segmentech krční a horních segmentech hrudní páteře. Cílem léčby je chirurgická radikální resekce cysty včetně jejího pouzdra. Autoři prezentují vzácnou kazuistiku a přehled dosud publikovaných obdobných případů.
Klíčová slova:
neurenterická cysta – kraniocervikální junkce – komprese míchy – enterogenní cysta – spinální dysrafizmus
Authors:
M. Bolcha 1; R. Bartoš 1; L. Mrázková 2; M. Sameš 1
Authors place of work:
Masaryk Hospital, Ústí nad Labem, Czech Republic
Department of Neurosurgery, JE Purkyně University
1; Masaryk Hospital, Ústí nad Labem, Czech Republic
Department of Radiology
2
Published in the journal:
Cesk Slov Neurol N 2012; 75/108(3): 363-367
Category:
Kazuistika
Summary
A neurenteric cyst (NEC) is a very rare diagnosis. These congenital lesions are defined as cysts lined by mucin-secreting epithelium, resembling that of the gastrointestinal tract. A neurenteric cyst can develop anywhere along the neuraxis, although it is predominantly found at the lower cervical and upper thoracic spinal level. The goal of surgical treatment is complete excision of the cyst, including its capsule. The authors present a case report and a review of all published similar cases.
Key words:
neurenteric cyst – craniocervical junction – medullary compression – enterogenous cyst – spinal dysraphism
Introduction
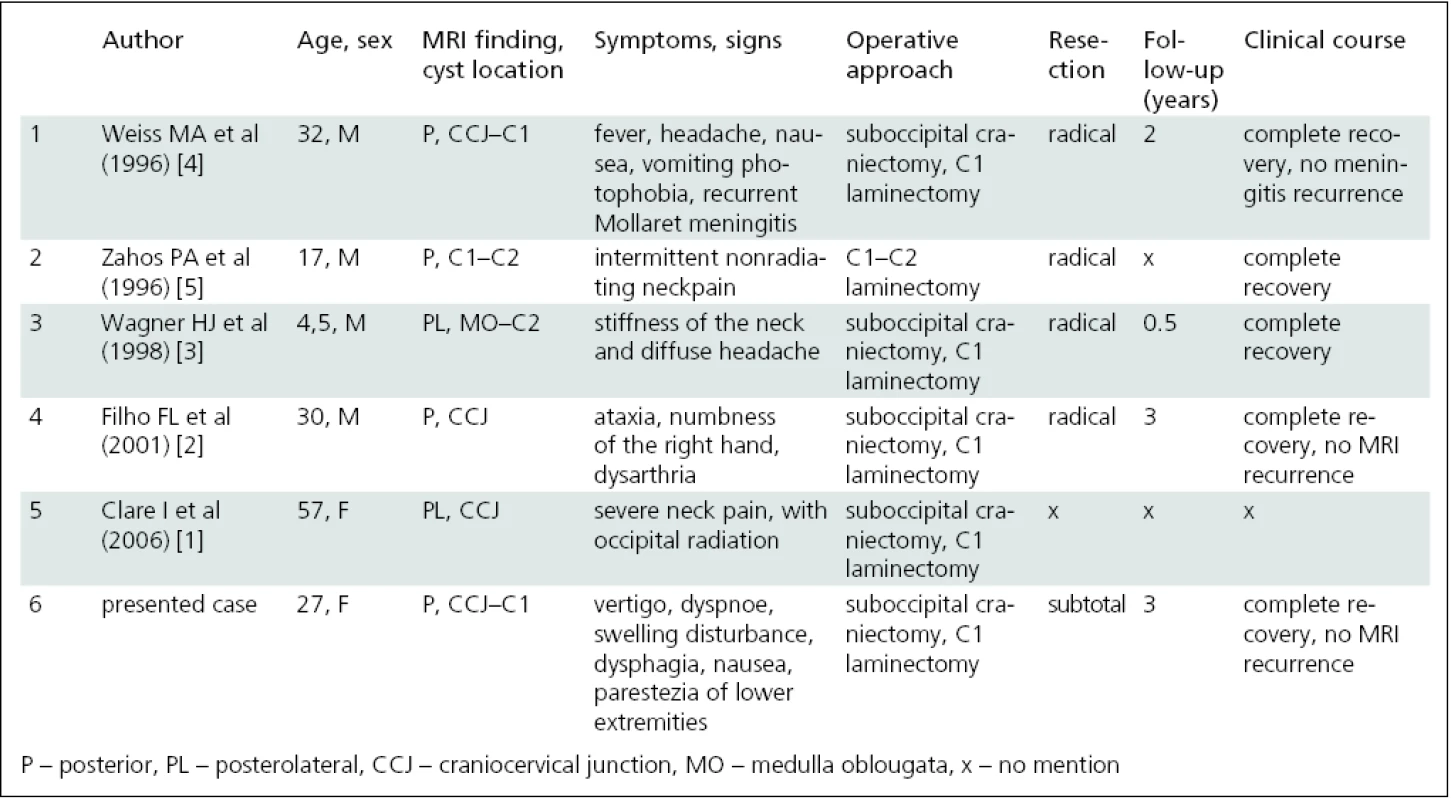
English-written publications report no more than 26 histologically verified neurenteric cysts in the high cervical region, including the craniocervical junction (CCJ). Only five of these were located dorsally to the spinal cord. The authors report an exceptional case of a neurenteric cyst posterior to the medulla oblongata of the craniocervical junction, the first case published in the Czech literature. An overview of all published cases of a dorsally located neurenteric cyst of the craniocervical junction is also presented (Tab. 1) [1–5].
Case report
Presentation and examination
A 27-year-old woman presented with a three months history of vertigo, cervicalgia, cephalgia, dyspnoe, dysphagia and nausea with intermittent vomiting. Later paresthesia of the lower limbs appeared without weakness. She was hospitalized several times because of these symptoms, all of which increased in severity over time.
Computer tomography (CT) showed a spherical cystic lesion of a density similar to that of the cerebrospinal fluid (CSF) dorsal to the medula oblongata with no associated spinal abnormalities. Magnetic resonance imaging (MRI) of the cervical spine revealed an unusual intradural extramedullar expansive lesion at the level of the craniocervical junction. The lesion was situated dorsolaterally, paramedially right from the medulla oblongata with mild pressure on the medulla. The size of the lesion was craniocaudal 24 mm, laterolateral 20 mm, sagittal 13 mm. MRI showed a very well bound lesion, slightly hyperintensive compared to the CSF on T1-weighted as well as T2-weighted imaging, iso-intensive with the CSF in flair mode. Postcontrast images showed no enhancement, and the spinal cord was without a myelopathic signal (Fig. 1a, b).

Upon admission to our department, the patient was conscious, well oriented, with cervicalgia and cephalgia. The patient had no cranial nerve lesion, speech disturbance or bulbar dysfunction. She also had no motor weakness or sensory deficit.
Surgery and histology
The patient underwent small posterior fossa craniectomy as far as the foramen magnum and C1 laminectomy in a semi-sitting position. During the operation, neuromonitoring of the XI cranial nerve, MEP and SSEP was performed. Durotomy up to C2 and opening of the cisterna magna disclosed a quite large, grayish, spherical cystic formation overlaid by a layer of the arachnoid. The cyst was released from both PICA, caudally from the CN XI that was stimulated and intact. The cyst adhered to the medulla oblongata and the vertebral arteries. Finally, a successful near radical resection from the medulla was made, although a thin layer remained on the vertebral arteries. A milky fluid was aspirated from the cyst.
Histopathological examination showed a cystic lesion lined with intestine-like epithelium, suddenly replaced with ciliated respiratory epithelium with goblet cells. Slightly squamous epithelium was also identified. Subepithelially, there was a thin layer of fibrous tissue and more pronounced meningothelial reactive hyperplasia with psammomatous-type calcifications. The histological diagnosis was an endodermal (neurenteric) cyst (Fig. 2, 3).


Postoperative course
The postoperative course was uneventful. At the time of discharge, the patient was without any symptoms. Two months after the surgery, the patient reported a return of moderate limb paresthesia and vertigo related to changes in the weather. Three years after surgery, MRI examination indicated a radical resection without any recurrence (Fig. 1c, d). The patient was asymptomatic.
Discussion
Definition, pathogenesis, epidemiology
A neurenteric cyst is defined as „a congenital malformation of the central nervous system and adjacent structures related to defective neural tube closure during the first trimester of pregnancy generally occurring between days 18–29 of gestation. Ectodermal and mesodermal malformations (mainly involving the skull and vertebrae) may occur as a result of defects of the neural tube closure“ [6]. An older WHO definition of the NEC is “a cyst lined by mucin-secreting epithelium, resembling that of the gastrointestinal tract” [7]. The first histologically verified neurenteric cyst was reported and termed “intestinoma” by Puusepp in 1934 [8]. Neurenteric cysts have been described using a variety of terms, such as an enterogenous or an enterogenic cyst [9,10]. At present, the term neurenteric cyst is most commonly used [6,10].
Many theories have been proposed to explain the origins of neurenteric cysts, either isolated or associated with complex malformations. All the theories are variations on a common theme of anomalous endodermal-ectodermal adhesion in the early embryonic life – known as the split notochord syndrome [11,12]. The mesoderm, lying along the midline of the embryo, forms the notochord. During the third gestational week, the notochord transiently intercalates itself into the endoderm, bringing it into contact with the yolk sac. Simultaneously, the neurenteric canal is also formed as a passage from the primary node in the ectoderm through the notochord to the endoderm, thus temporarily connecting the amniotic cavity with the yolk sac [10–12]. Persistence of this canal may interfere with the notochord development and result in the formation of a neurenteric cyst. Adhesions between the notochord and the endoderm may be associated with spina bifida and, extremely rarely, with the developement of dorsal enteric fistula [11,12].
A neurenteric cyst may develop anywhere along the neuraxis. It is found predominantly at the lower cervical and upper thoracic spinal level, with a lower incidence at the lumbar and sacral levels [13]. In very rare cases, a neurenteric cyst may occur at the craniocervical junction, the cerebellopontine angle, the brainstem or in a brain hemisphere [10,14,15]. In the majority of cases, a spinal canal neurenteric cyst develops intradurally-extramedullary and ventrally to the spinal cord. NEC can be also associated with spinal anomalies [9,10,12,16].
Occurrence of NEC is more frequent in men than in women in a ratio of 2 : 1 [9].
Histology
Histologically, a thin-walled cyst is the most common type of a neurenteric cyst, lined by a layer of pseudostratified, stratified cuboidal or columnar epithelium lying on a basement membrane. The cyst is supported by a connective tissue wall with variable vascularity. The epithelial cells may or may not be ciliated. Frequently found are mucin-secreting, PAS reaction-positive goblet cells that are thought to be responsible for the growth of the cyst [16]. Imunohistochemical staining shows cytokeratin CAM 5.2, EMA (epithelial membrane antigen) and CEA (carcinoembryonic antigen) positivity. Conversely, neurenteric cysts are mostly GFAP (glial fibrillary acidic protein), vimentin and S-100 negative [16,17].
Ependymal cysts should be mentioned as part of histological differential diagnosis of intradural epithelial cysts; they are distinguished by GFAP positivity, no cytokeratin and little or no glycoprotein in the cytoplasm of their epithelial cells [18].
Symptoms, imaging and differential diagnosis
Symptoms usually occur during childhood or in early adult life, most often during the second or third decade of life. Review of cases shows an average patient age of approximately 28 years (Tab. 1) [1–5]. The characteristic symptoms of a NEC in the CCJ include headache, mainly occipital, nuchal spasms and, frequently, severe neck pain. Cerebellar signs, palsy of the cranial nerves and paresis of extremities may also be seen (Tab. 1) [1–5]. In one patient, neurenteric cyst was caused by recurrent Mollaret meningitis [4].
MRI is the imaging modality of choice [10,12]. It provides valuable information about the nature of the cyst, including its location and signal relative to the CSF as well as its relationship with other structures, thus assisting the surgeon in planning the best surgical approach [14,15]. MRI shows NECs to be isointense to hyperintense relative to the CSF in T1-weighted images and isointense or slightly hyperintense compared to the CSF in T2-weighted images. This MRI signal characteristic results from the high protein content of the NEC, described as milky or mucinous by surgeons [10,14]. Absence of contrast enhancement and mural nodule differentiates a NEC from neoplastic lesions. CT scanning can be helpful in finding associated bone abnormalities but it may fail in visualizing the craniocervical junction.
Differential diagnosis of intraspinal cystic mass structures includes an arachnoid cyst, a dermoid cyst, an epidermoid cyst, a teratoma, a parasitic cyst, an ependymal cyst, cystic cord tumors, a cystic meningeoma, and postinflammatory or posttraumatic arachnoid cysts [19].
Therapy
Treatment of neurenteric cysts involves surgical excision of the cyst, including its capsule. An approach is selected depending on the location of the cyst. Dorsally located NECs are commonly resected using the posterior approach, as was the case in our patient [1–5].
Whenever possible, total removal of the cyst is recommended. However, it may be identified during the surgery that the cyst wall strongly adheres to surrounding neurovascular structures, in which case only subtotal extirpation is possible [1,2]. It is generally agreed in the literature that partial removal is efficacious [20].
There is no correlation between recurrence of the cyst and other factors such as age, location, sex, or size. The only factor that leads to recurrence of the cyst is partial resection [18]. Results of radical surgical treatment are excellent and recurrence is very rare [1–5, 20]. Careful radiological follow-up should be performed.
Conclusions
A neurenteric cyst is a very rare lesion with a very good prognosis, given timely diagnosis. MRI is a gold standard imaging method for neurenteric cysts. The characteristic symptoms of a NEC in the CCJ are headache, mainly occipital, nuchal spasms and, frequently, severe neck pain. Cerebellar signs, palsy of the cranial nerves and paresis of extremities can also be seen. The first choice approach to a posteriorly located NEC in a craniocervical junction is suboccipital craniotomy and C1 laminectomy. Clinical course in the majority of patients showed complete recovery without recurrence, even following subtotal resection.
Acknowledgments: Ivana Julišová, MD, PhD, Biolab Praha s.r.o, bioptic, histochemical and cytological laboratory, Prague, Czech Republic, for histology and histological figures.
Martin Bolcha, M.D.
Masaryk Hospital, Department of Neurosurgery
Sociální péče 3316/12A
401 13 Ústí nad Labem
e-mail: martin.bolcha@mnul.cz
Accepted for review: 17. 6. 2010
Accepted for publication: 3. 10. 2011
Zdroje
1. Clare I, Kavar B, Dobie P. Neurenteric cyst of the craniocervical junction. Australas Radiol 2006; 50(1): 59–62.
2. Filho FL, Tatagiba M, Carvalho GA, Weichhold W, Klekamp J, Samii M. Neurenteric cyst of the craniocervical junction. Report of three cases. J Neurosurg 2001; 94 (Suppl 1): 129–132.
3. Wagner HJ, Seidel A, Reusche E, Sepehrnia A, Kruse K, Sperner J. A craniospinal enterogenous cyst: case report. Neuropediatrics 1998; 29(4): 212–214.
4. Weiss MA, Gebarski SS, McKeever PE. Foramen magnum neurenteric cyst causing mollaret meningitis: MR findings. AJNR Am J Neuroradiol 1996; 17(2): 386–388.
5. Zahos PA, Goodman LA, Onesti ST, Michelsen WJ. Dorsal endodermal cyst of the upper cervical spine. J Spinal Disord 1996; 9(6): 536–539.
6. Joynt RJ. Clinical Neurology. Philadelphia: Lippincott 1992: 31–41.
7. Zülch KJ. Histological typing Of tumours of the central nervous system. Geneva: World Health Organization 1979.
8. Puusepp M. Variété rare de tératome sous-dural de la région cervicale (intestinome). Quadriplégie. Extirpation. Guérison compléte. Rev Neurol 1934; 2: 879–886.
9. Agnoli AL, Laun A, Schönmayr R. Enterogenous intraspinal cysts. J Neurosurg 1984; 61(5): 834–840.
10. Brooks BS, Duvall ER, el Gammal T, Garcia JH, Gupta KL, Kapila A. Neuroimaging features of neurenteric cysts: analysis of nine cases and review of the literature. AJNR Am J Neuroradiol 1993; 14(3): 735–746.
11. Macdonald RL, Schwartz ML, Lewis AJ. Neurenteric cyst located dorsal to the cervical spine: case report. Neurosurgery 1991; 28(4): 583–587.
12. Menezes AH, Traynelis VC. Spinal neurenteric cysts in the magnetic resonance imaging era. Neurosurgery 2006; 58(1): 97–105.
13. Rodacki MA, Teixeira WR, Boer VHT, Caropreso J, Oliveira GG. Intradural, extramedullary high cervical neurenteric cyst. Neuroradiology 1987; 29(6): 588.
14. Chaynes P, Thorn-Kany M, Sol JC, Arrué P, Lagarrigue J, Manelfe C. Imaging in neurenteric cysts of the posterior cranial fossa. Neuroradiology 1998; 40(6): 374–376.
15. Kimura H, Nagatomi A, Ochi M, Kurisu K. Intracranial neurenteric cyst with recurrence and extensive craniospinal dissemination. Acta Neurochir (Wien) 2006; 148(3): 347–352.
16. Fuse T, Yamada K, Kamiya K, Inagaki H. Neurenteric cyst at the craniovertebral junction: report of two cases. Surg Neurol 1998; 50(5): 431–436.
17. Mackenzie IR, Gilbert JJ. Cysts of the neuraxis of endodermal origin. Neurol Neurosurg Psychiatry 1991; 54(7): 572–575.
18. Breeze RE, Nichols P, Segal H, Apuzzo ML. Intradural epithelial cyst at the craniovertebral junction. Case report. J Neurosurg 1990; 73(5): 788–791.
19. Friedburg H, Schumacher M, Hennig J. Pathology of the craniocervical junction as shown by magnetic resonance tomography. 68 cases. Fortschr Röntgenstr 1986; 145(3): 315–320.
20. Kim CY, Wang KC, Choe G, Kim HJ, Jung HW, Kim IO et al. Neurenteric cyst: its various presentations. Child‘s Nerv Syst 1999; 15(6–7): 333–341.
Štítky
Dětská neurologie Neurochirurgie NeurologieČlánek vyšel v časopise
Česká a slovenská neurologie a neurochirurgie

2012 Číslo 3
Nejčtenější v tomto čísle
- Neurosyphilis
- Surgical Treatment of a Tarsal Tunnel Syndrome
- Bilateral Phrenic Nerve Lesion Manifesting as an Orthopnea – Three Case Reports
- Diagnosis and Treatment Options for Niemann-Pick Disease Type C
